Simple bone cyst
Clinical History
A 13-year-old female presented with a radiolucent lesion apical to teeth #18 and 19 which were vital. The lesion appeared associated with impacted tooth #17. There was no mandibular expansion present and no bone perforation. Aspiration revealed semiclear fluid (courtesy of Dr. Nick Spanel, Oral Surgeon).
Radiographic features
The orthopantomogram (Figure 1) reveals radiolucency in the posterior left area of the mandible with scalloping superior aspect between the roots of the left mandibular molars. The differential diagnosis can include simple (so-called traumatic) bone cyst, ameloblastoma or keratocystic odontogenic tumor (odontogenic keratocyst). Upon surgical entry (Figure 2) minimal intramedullary tissue was identified.
Figure 1

Figure 2

Histopathologic features
Submitted tissues were characterized by loose vascular fibrocollagenous connective tissue with areas of hemorrhage and fragments of woven bone (Figures 3&4) with basophilic lace-like pattern of calcification (Figure 5).
Figure 3
Scattered fragments of loosely collagenized connective tissue with hemorrhage and woven bone spicules with lace-like or lattice like calcifications.
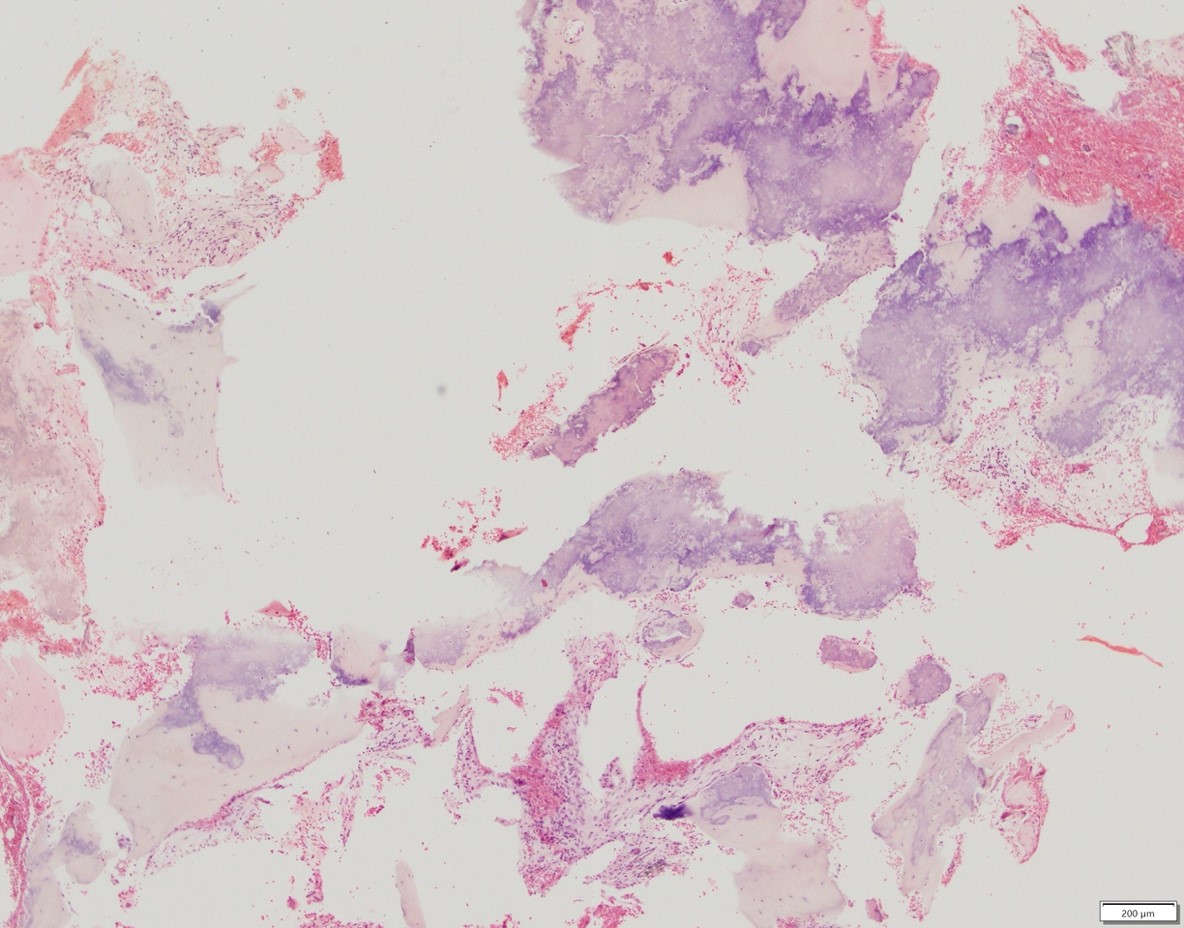
Figure 4
Higher power features loose fibrocollagenous connective tissue, hemorrhage and calcifications with lace-like or lattice-like pattern.
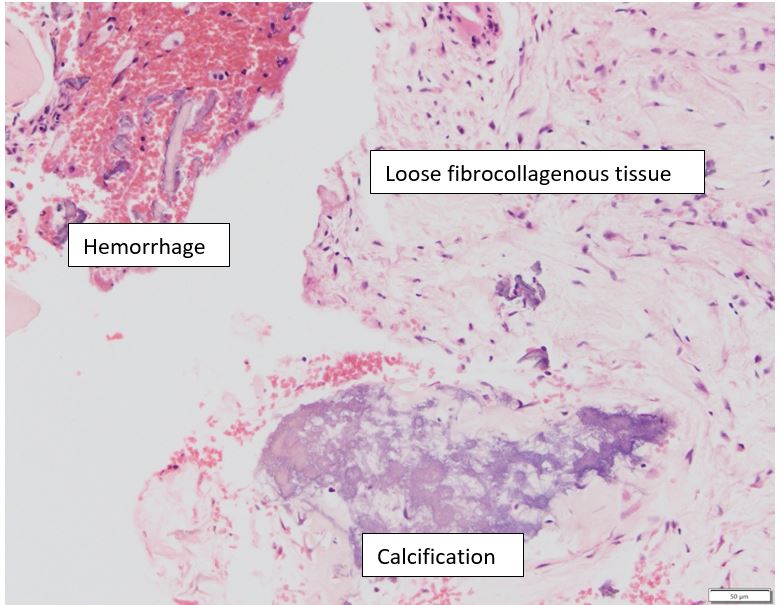
Figure 5

Diagnosis
Simple bone cyst
Treatment
Surgical exploration with curettage
Discussion
Simple (so-called traumatic; hemorrhagic; solitary; unicameral) bone cyst is a generally empty or fluid-filled bone cavity with limited amount of tissue and without epithelial lining. The lesion is also known as traumatic bone cyst since the trauma-hemorrhage theory has been used to explain the etiology. However, not all cases are associated with trauma. Therefore, the term simple bone cyst is preferred, at least by us, at the University of Minnesota.
Simple bone cysts can occur in any bone of the skeleton. When it comes to jaws the vast majority of cases affect the mandible. We have encountered examples in the maxilla, but they are very rare and the diagnosis for maxillary lesions is rendered only if all possible other diagnostic possibilities are excluded. There is no gender predilection when it comes to the jaws, however, males are more frequently affected in extragnathic sites. Most patients are children and adolescence. Gnathic cases are asymptomatic with 15-20% patients presenting with slight enlargement. In contrast to the jaws, lesions of the long bone have aggressive behavior.
Occasionally, simple bone cysts may be seen in association with impacted third molars and benign fibro-osseous lesions.
Osteoscarcoma
Clinical History
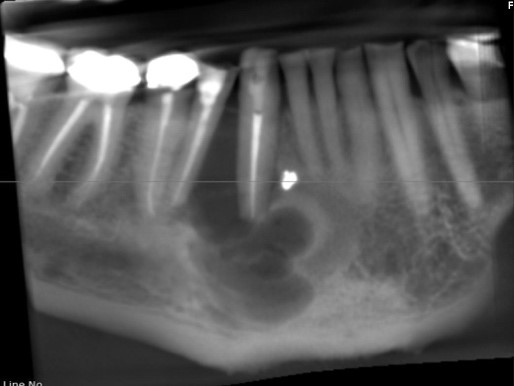
A 20 y/o female, who is 24 weeks pregnant, presented for evaluation of right submandibular and sublingual swelling along with V3 paresthesia associated with partially erupted #32. A 4-month old panoramic radiograph showed no overt radiolucency (Figure 1). The third molar was extracted for presumed pericoronitis. Upon extraction of the tooth significant abnormal tissue was noted apical and mesial to #32 area. A new panoramic radiograph was taken (Figure 2) which reveals moth eaten bone in right mandible and root resorption associated with #31. An incisional biopsy was taken with the lesions being suspicious for osteomyelitis versus osteosarcoma (Courtesy of Dr. Tyler Varhol, Oral Surgeon)
Radiographic features
The radiograph in Figure 1 features partially erupted right third mandibular molar. Subtle radiopacity is present on the distal aspect of the mesial root of tooth #31.
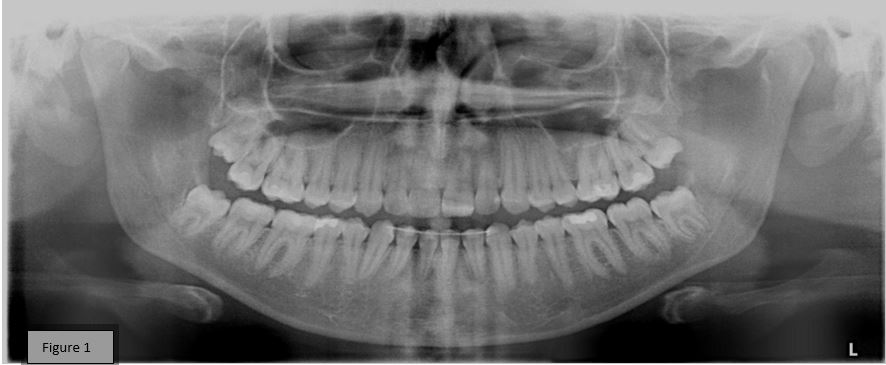
Figure 2 reveals larger radiopacity on the distal aspect of the mesial root of tooth #31 with associated root resorption, as well as mixed lucent and opaque variations in association with tooth #32 and extending proximally to tooth #30 and distally to tooth #31.

Histopathologic features
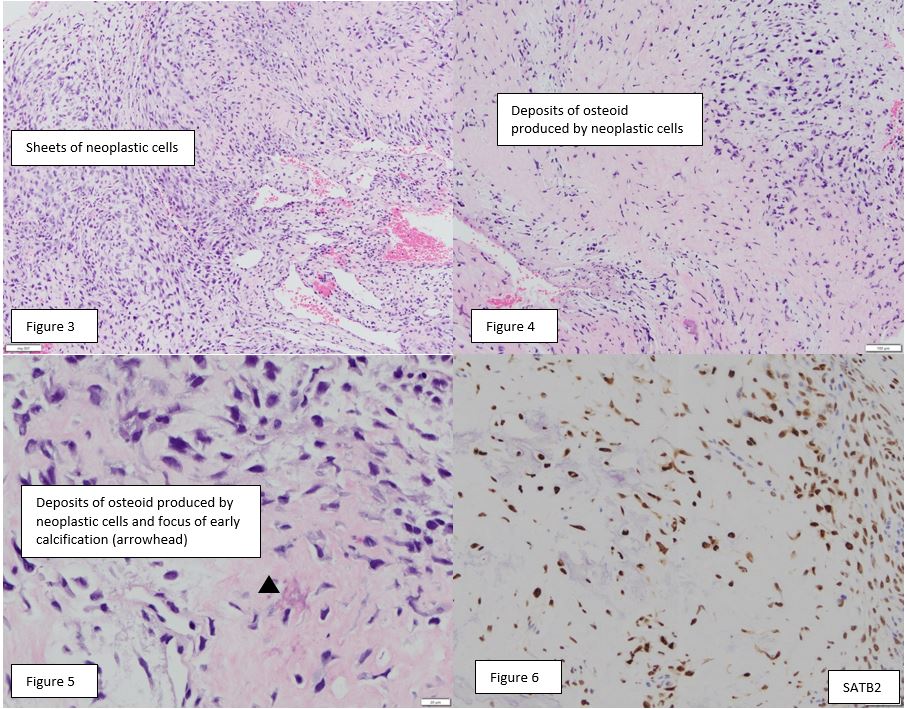
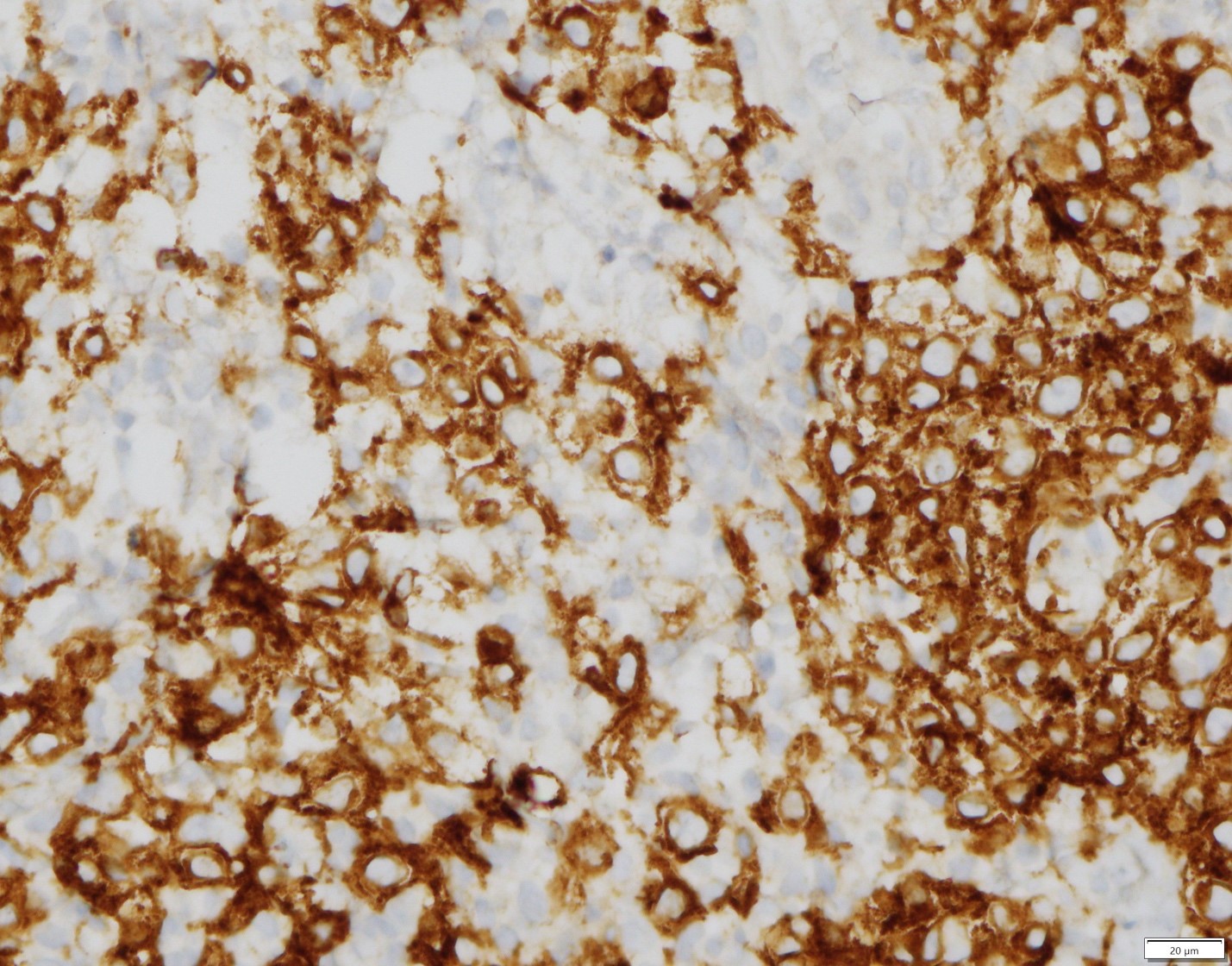
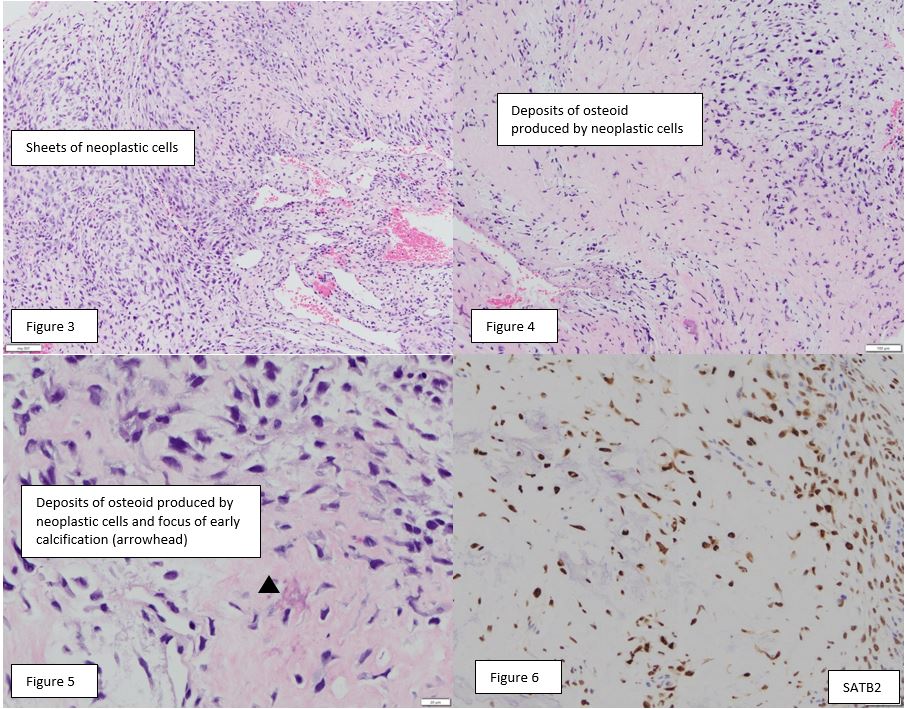
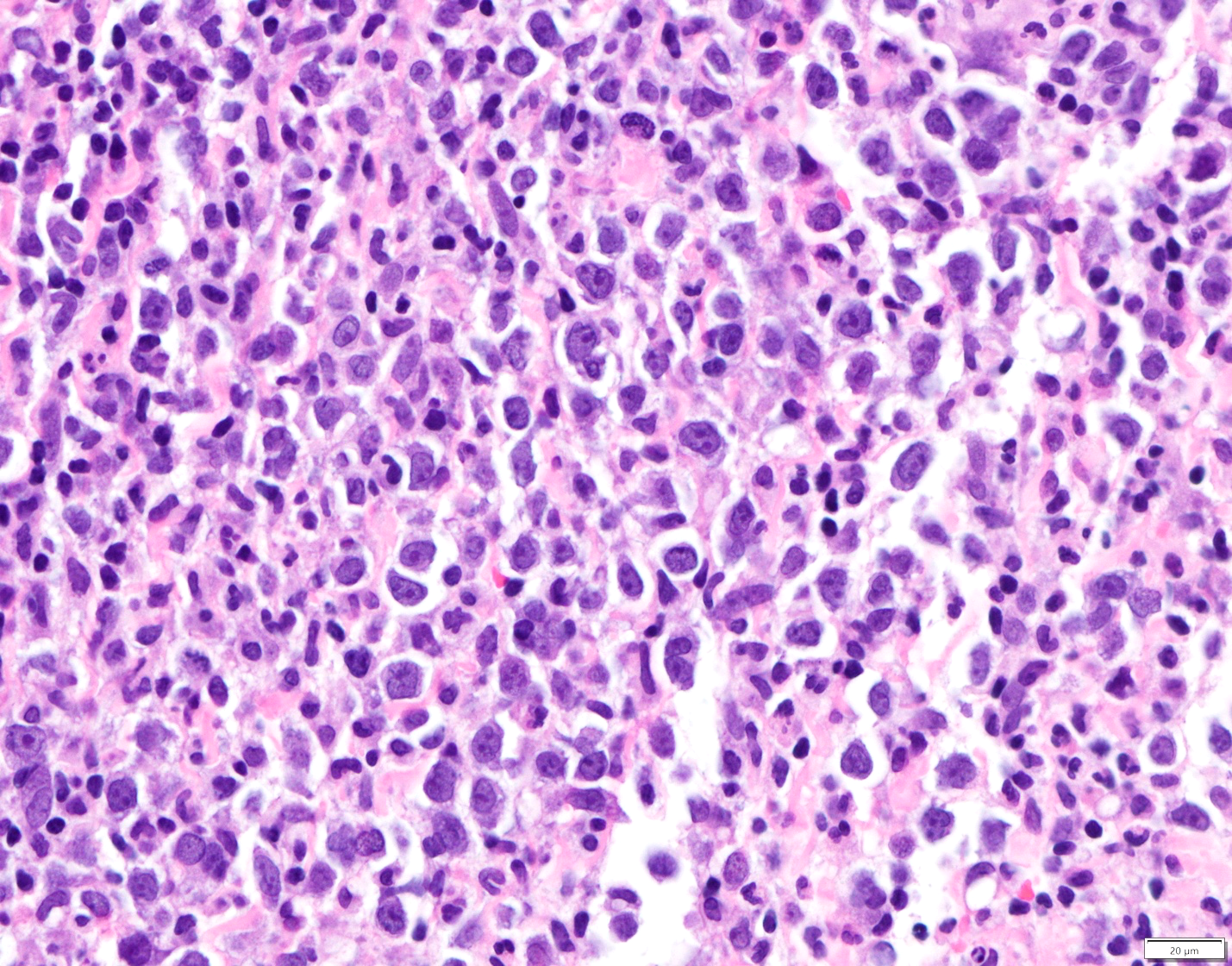
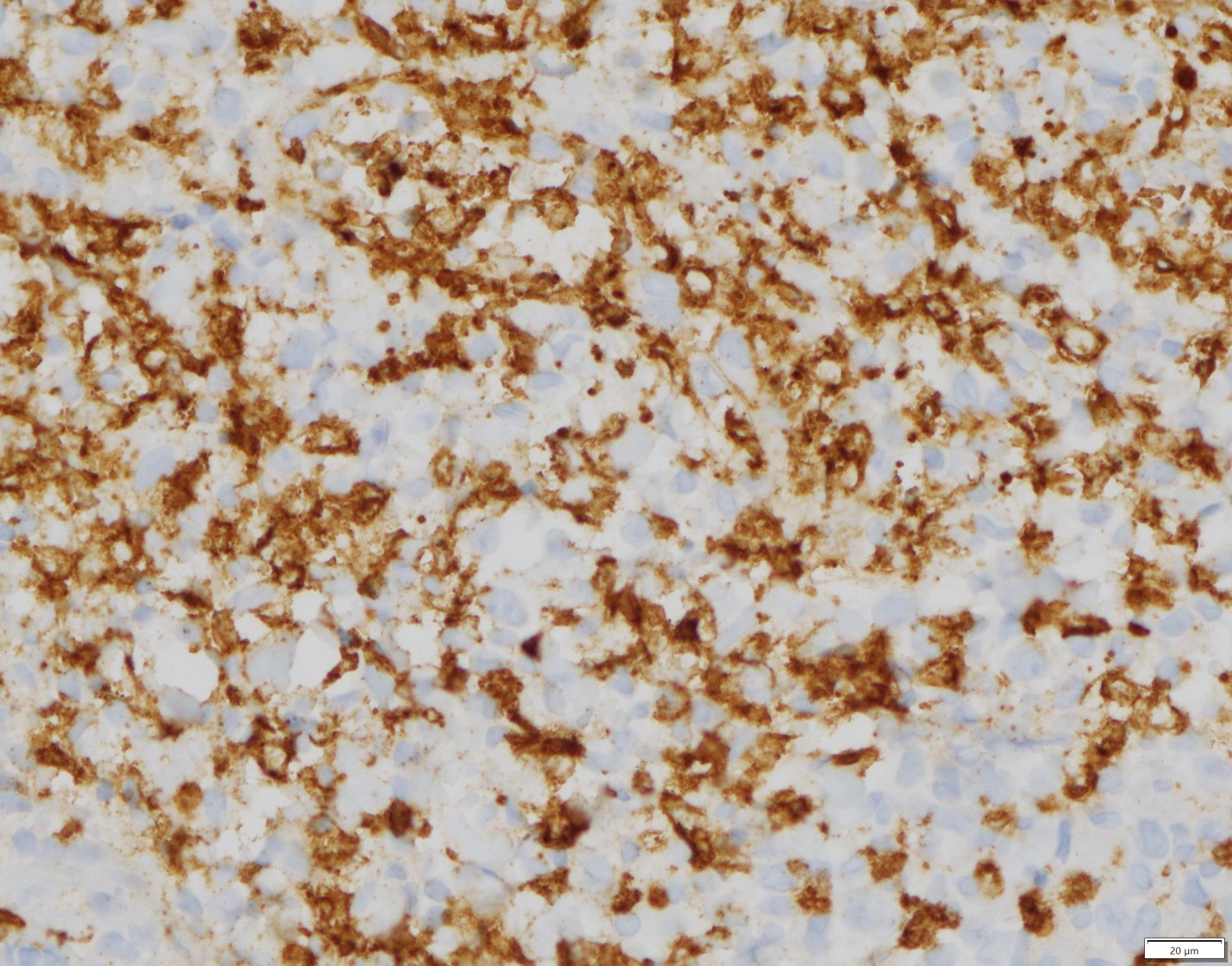
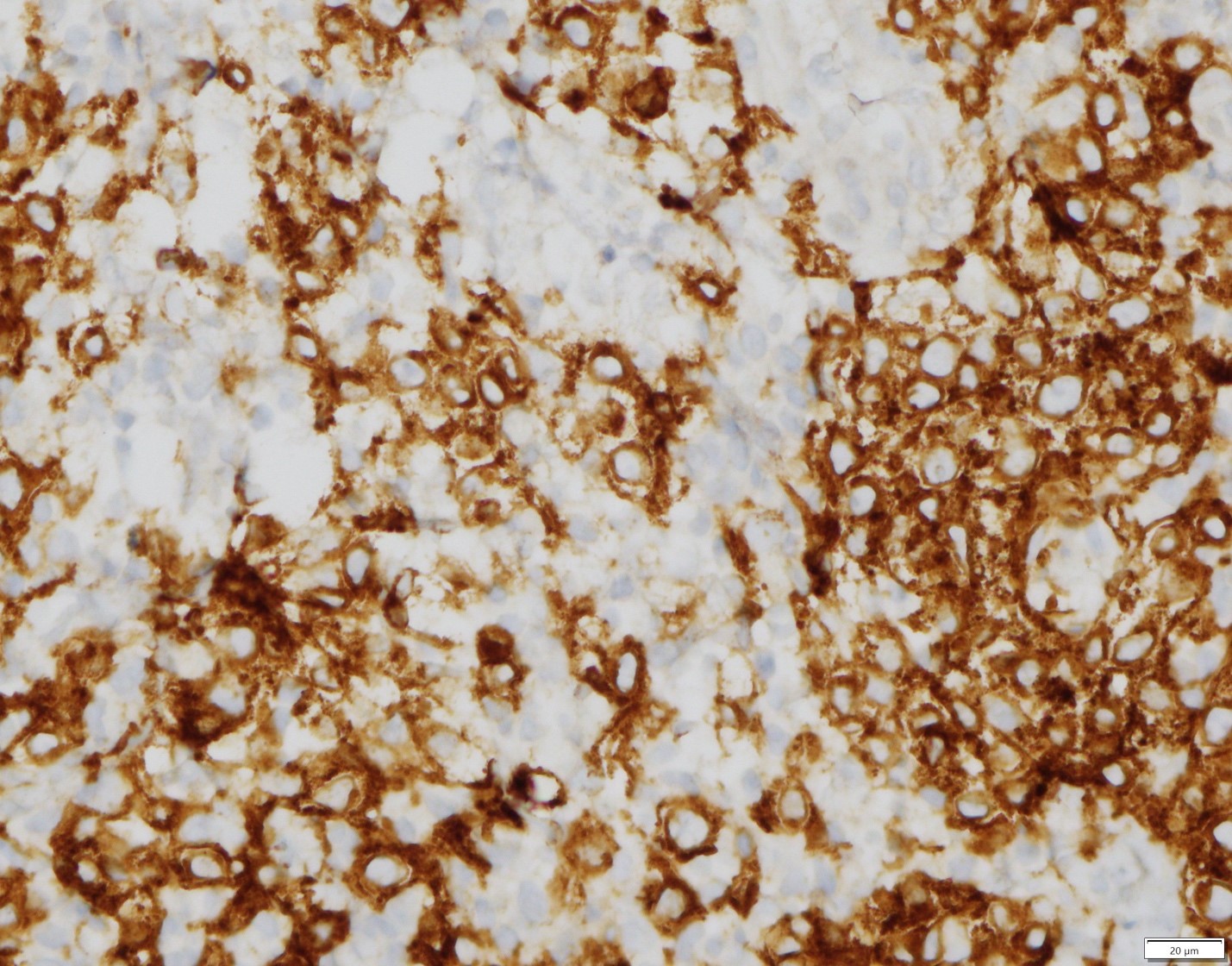
Incisional biopsy revealed proliferation of sheets (Figure 3) of predominantly spindle cells exhibiting spindle or ovoid hyperchromatic nuclei and spindle cytoplasm (Figures 4&5). Individual cells featured pleomorphism and mitoses. These neoplastic cells formed osteoid (Figure 4&5) with foci of calcifications (Figure 5). The stroma was characterized by increased vascularity. A special immunohistochemical stain, SATB2 (Figure 6), a transcriptional regulation and chromatin remodeling DNA binding protein, decorated neoplastic cells.
Diagnosis
Osteoblastic osteosarcoma
Discussion
Osteosarcoma of the jaws is a rare form of sarcoma. There are three major types of osteosarcoma and all three can affect the jaws. These types are central, surface and extraskeletal. Central osteosarcoma is the most common of the three and has three major subtypes, osteoblastic, chondroblastic and fibroblastic. There are some rarer forms also, i.e. telangiectatic, small cell, osteoblastoma-like, etc. The surface or juxtacortical type has three subtypes, parosteal, periosteal and high-grade surface. The present type is central osteoblastic.
Radicular cyst and CGCL
Clinical History
A 73-year old male presented on 01/19/2019 for routine dental care when a draining lesion was noted on clinical examination in the maxilla (Courtesy of Dr. Brett Moore, Plymouth MN).
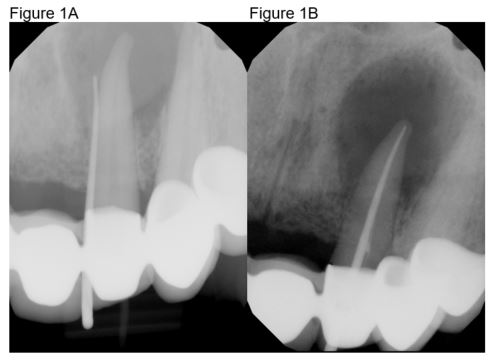
Radiographic features
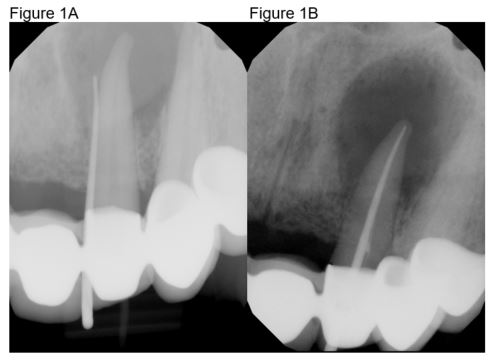
The lesion was traced to the apex of tooth #10 which was associated with a radiolucent lesion (Figure 1A). The tooth was non-responsive to cold. Root canal treatment was completed on 1/23/2019 (Figure 1B). The patient went back to clinic in July 2019 with radiolucency appearing to heal but the sinus tract still present. The patient was referred to an endodontist but did not pursue the referral. The patient returned to clinic on 1/22/2020 with persistent sinus tract. He was given the option to go to an endodontist for evaluation or to amputate root to preserve the bridge with removal of cyst and grafting. The patient decided the latter and the surgical procedure was completed on 2/26/2020.
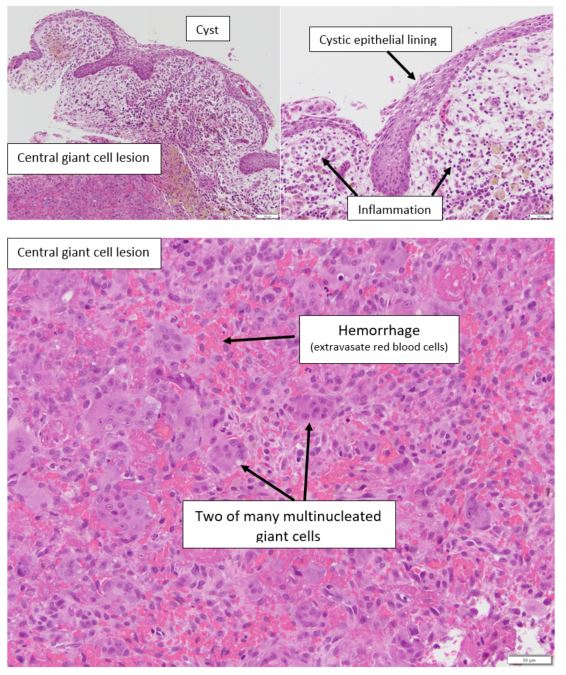
Histopathologic features
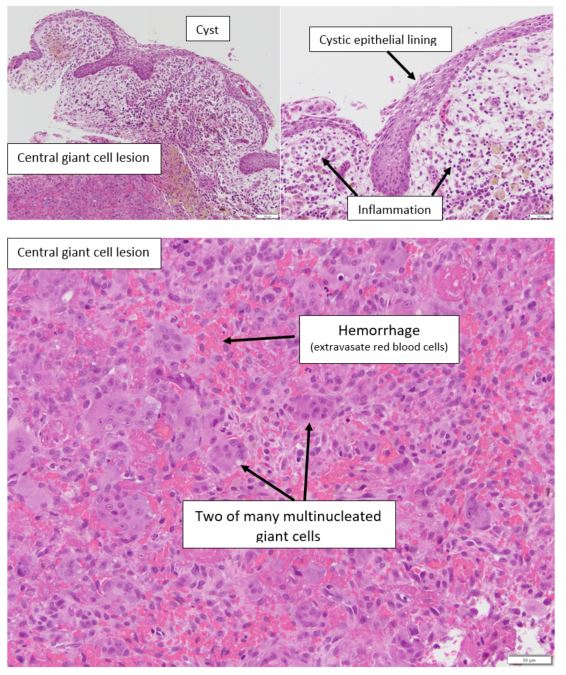
The specimen revealed an inflamed odontogenic cyst lined by non-keratinizing thin stratified squamous epithelium. In the wall of the cyst another process was present which was characterized by multiple fibroblasts and multinucleated giant cells in a hemorrhagic stroma.
Diagnosis
Central giant cell lesion and radicular cyst
Treatment
Excision with follow-up of the patient
Discussion
While radicular cyst is the most common odontogenic cyst of the jaws, central giant cell lesions are uncommon. Rarely, a giant cell lesion may be seen in association with another lesion in jaws, e.g. odontogenic cyst or odontogenic tumor like ameloblastoma. In the present case we cannot determine which came first, the cyst or the giant cell lesion. Regardless, the patient should be followed because giant cell lesions can recur. Another name that is issued for central giant cell lesion is central giant cell granuloma. When the diagnosis of central giant cell lesion is made, it is prudent to refer the patient to their physician for laboratory evaluation of calcium, phosphate and parathormone levels. Although in most instances central giant cell lesions are solitary without an underlying systemic cause, the possibility of hyperparathyroidism cannot be excluded by means of histopathology and radiology alone.
Congenital epulis
Clinical History
A 15-day-old female with slight nursing difficulty presented with an 1 cm in greatest dimension fibrous nodular lesion on the right anterior side of the maxillary alveolar ridge (Figure 1A). The lesion was present at birth and has become somewhat bigger. The lesion was excised (Courtesy of Dr. Chelsea Erickson, East Grand Forks, MN).

Radiographic features
The bone was not involved
Histopathologic features
Nodular lesion (Figure 1A) was surfaced by non-neoplastic thin parakeratinizing stratified squamous epithelium. In the connective tissue sheets of granular cells in a rich vascular stroma were present. There were also foci of mild inflammation.
Diagnosis
Congenital epulis (congenital granular cell lesion, congenital granular cell epulis)
Treatment
The lesion was excised and recurrence is not expected.
Discussion
Congenital epulis is seen primarily in female newborns with a female to male ratio approaching 10:1. Although there is such female predilection, lesions do not harbor progesterone or estrogen receptors. Lesions present as solitary polyps with the maxillary alveolar mucosa 2-3 more frequently affected than the mandibular. The histogenesis of the lesion is unknown but the possibility of an unusual odontogenic lesion cannot be ruled out. The size of the lesions is approximately 1-2 cm but larger lesions have been described causing difficulties in breastfeeding or using a baby bottle. Surgical excision is the treatment of choice although complete regression has been described in some patients with partial excision or even without any treatment.
Arteriovenous hemangioma
Clinical History
27-year-old female presented with non-raised erythematous lesion (arrow) on the palate 0.5 cm in greatest dimension which blanched when pressed. The lesion did not affect the bone (Courtesy of: Jason Leet, Resident in Oral Surgery and Madeleine Gamble, Orthodontics Resident in Orthodontics)
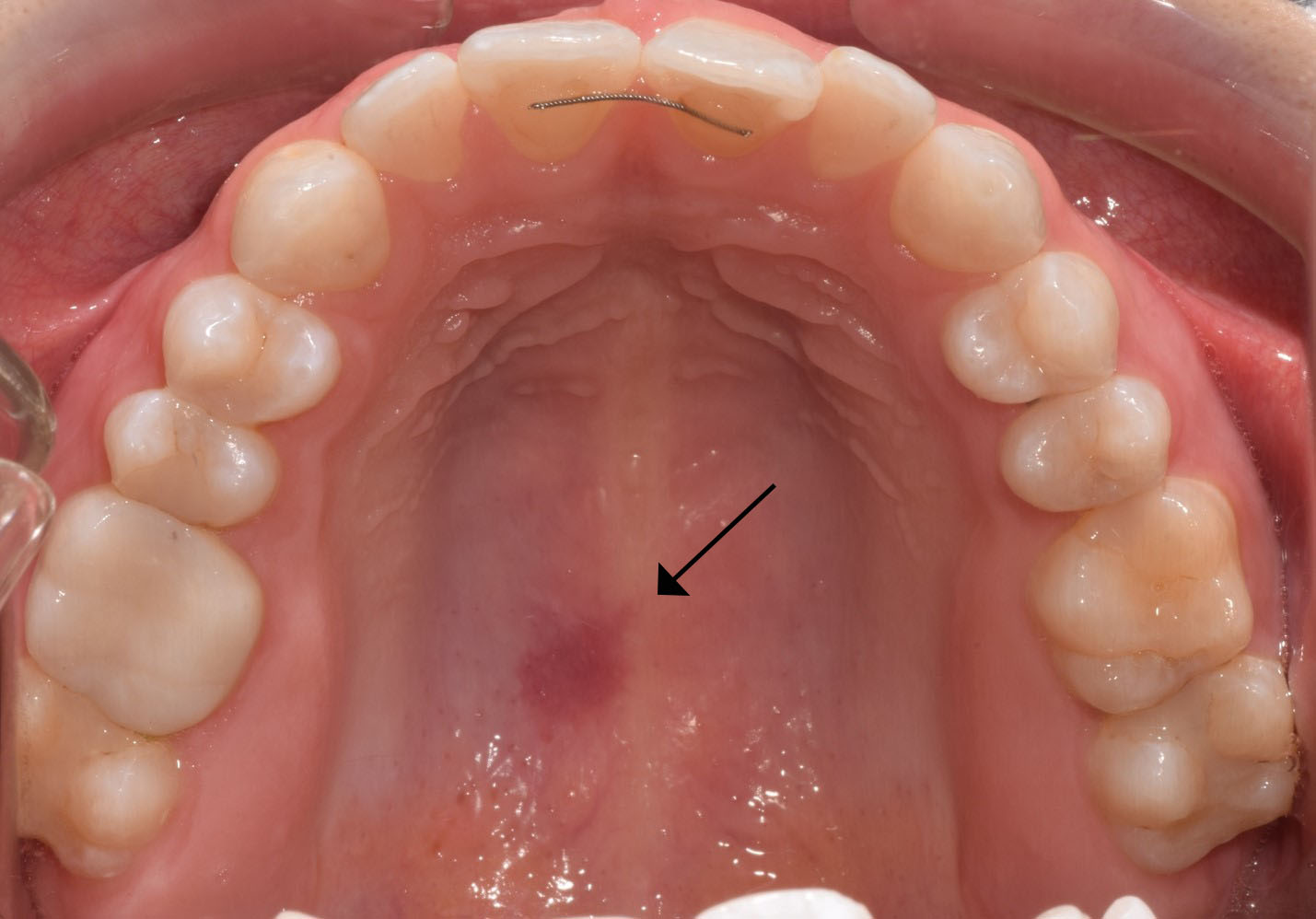
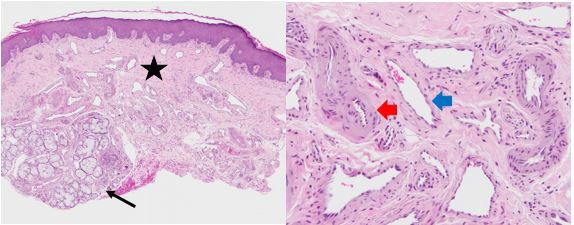
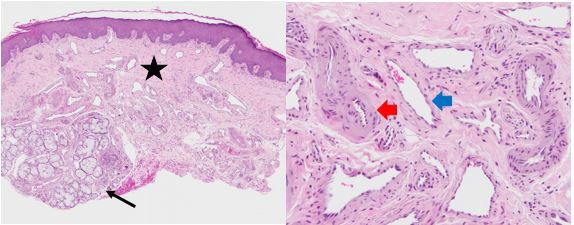
Histopathologic features
The mucosal fragment is covered by non-neoplastic keratinizing stratified squamous epithelium and reveals, in the lamina propria, multiple capillaries with occasionally conspicuous smooth muscle wall (star). These capillaries have properties of arterioles (red arrow) and venules (blue arrow). Included in the connective tissue are portions of mucous minor salivary glands (black arrow).
Diagnosis
Arteriovenous hemangioma (proliferation)
Treatment
The lesion was excised and the patient will be followed.
Discussion
Arteriovenous hemangioma (AVH) is an uncommon vascular proliferation seen on the lips, tongue, palate, gingiva and alveolar mucosa. Women are slightly more frequently affected than men. The lesions are generally small and can present either as nodules or as flat erythematous macules. In most instances, they are characterized by diffuse proliferation of capillaries with properties of arterioles and venules. The etiology is uncertain and trauma may be responsible for this vascular proliferation or malformation. Some lesions may be true hamartomas. Surgical excision is the treatment choice with approximately 11% recurrence rate.
Metastatic breast cancer to maxilla
Clinical History
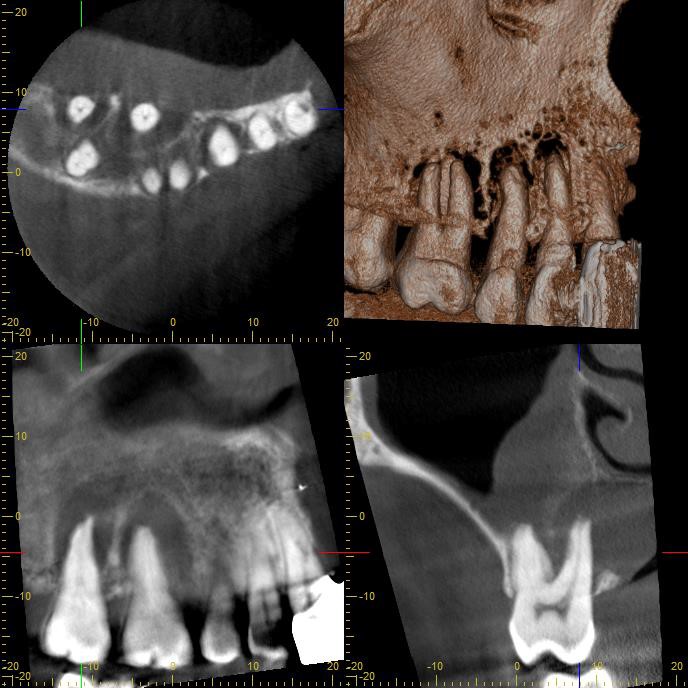
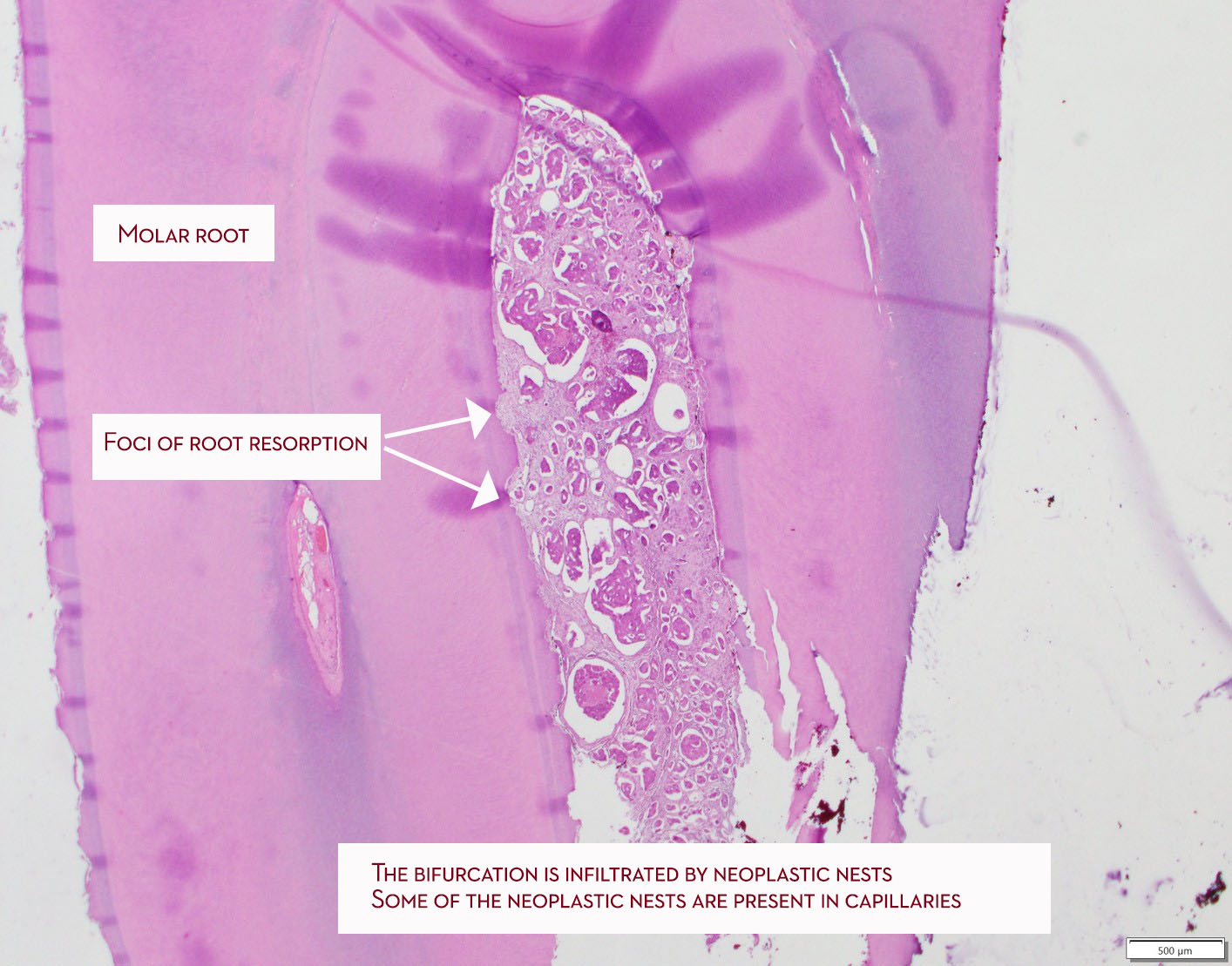
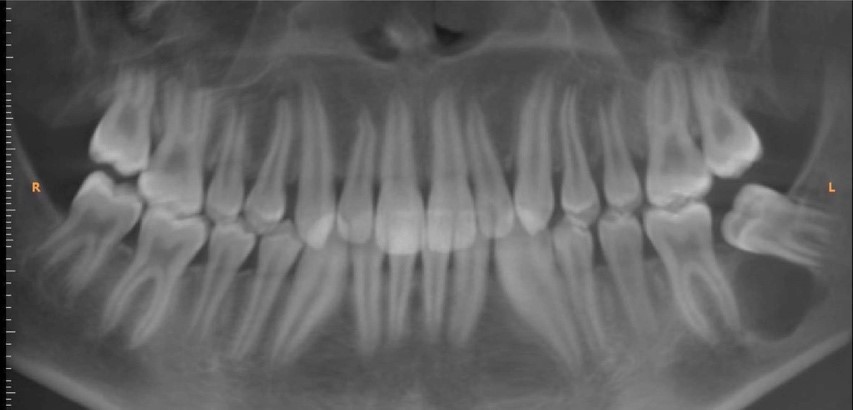
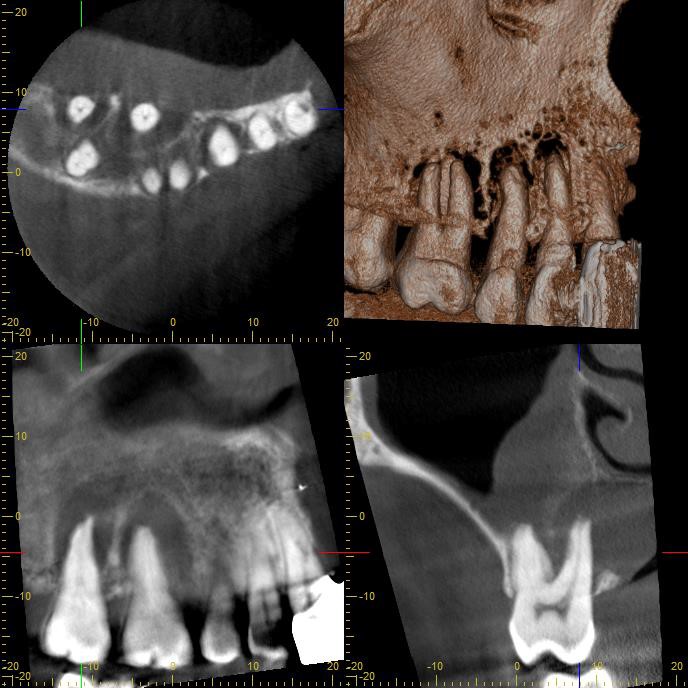
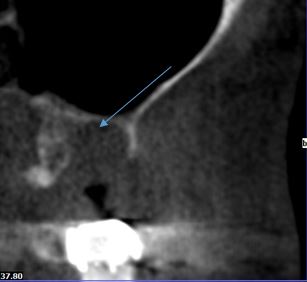
A 42-year-old female with history of breast cancer presented with rapid onset of bone loss associated with teeth # 2-5 which tested vital. There was no evidence of periodontal pockets. CBCT scan showed erosion of maxillary sinus floor and root resorption associated with at least tooth # 2. (Contributed by Dr. Dan Sampson, Oral Surgeon)
Radiographic features
The tumor presented with spiked dental root resorption and tumor affecting the right sinus.
Histopathologic features
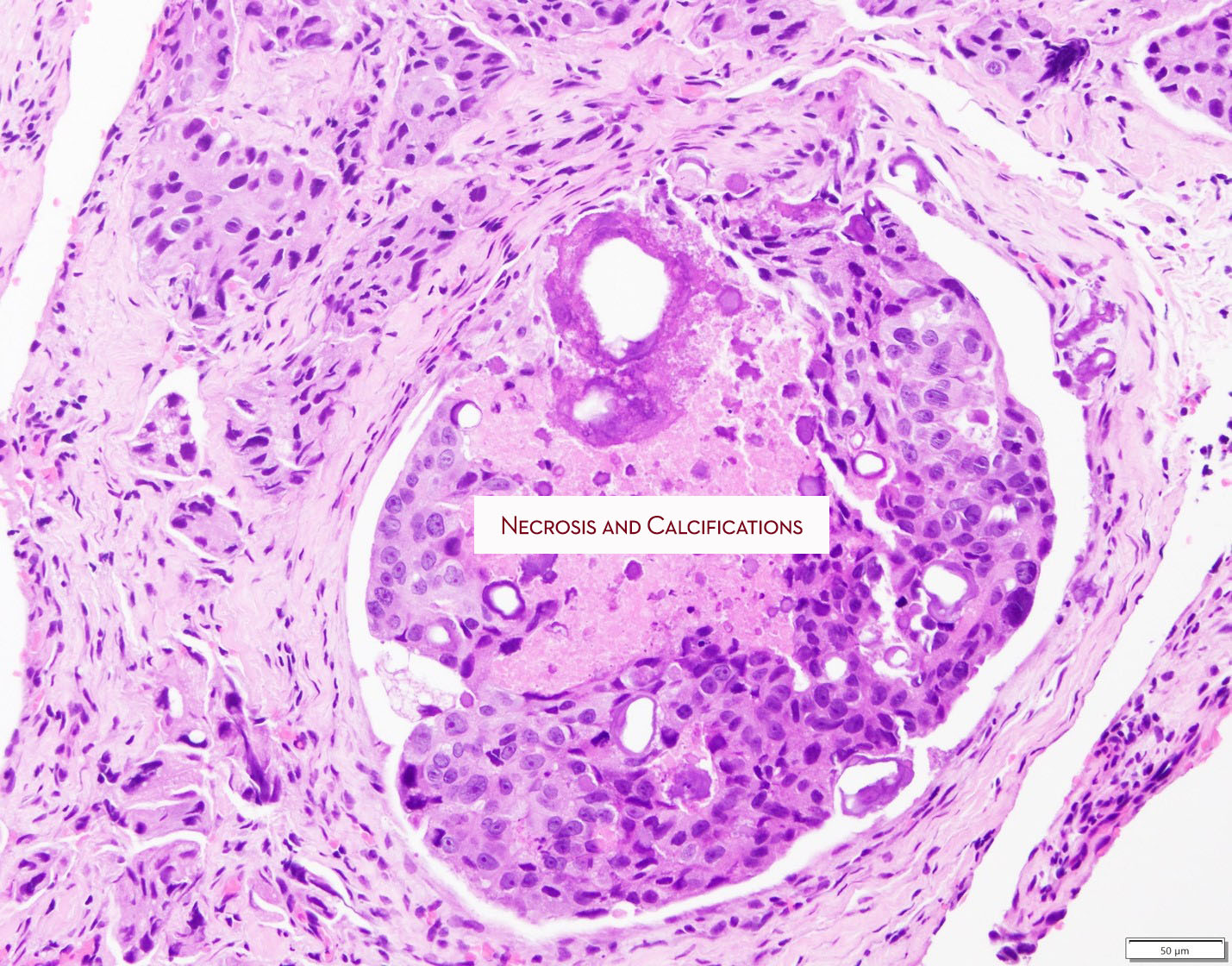
Nests of neoplastic cells of infiltrated the bone. Neoplastic cells vary in size and exhibit nuclear hyperchromatism and mitotic activity. Some of the nests feature necrosis of cells and there are dystrophic calcifications.
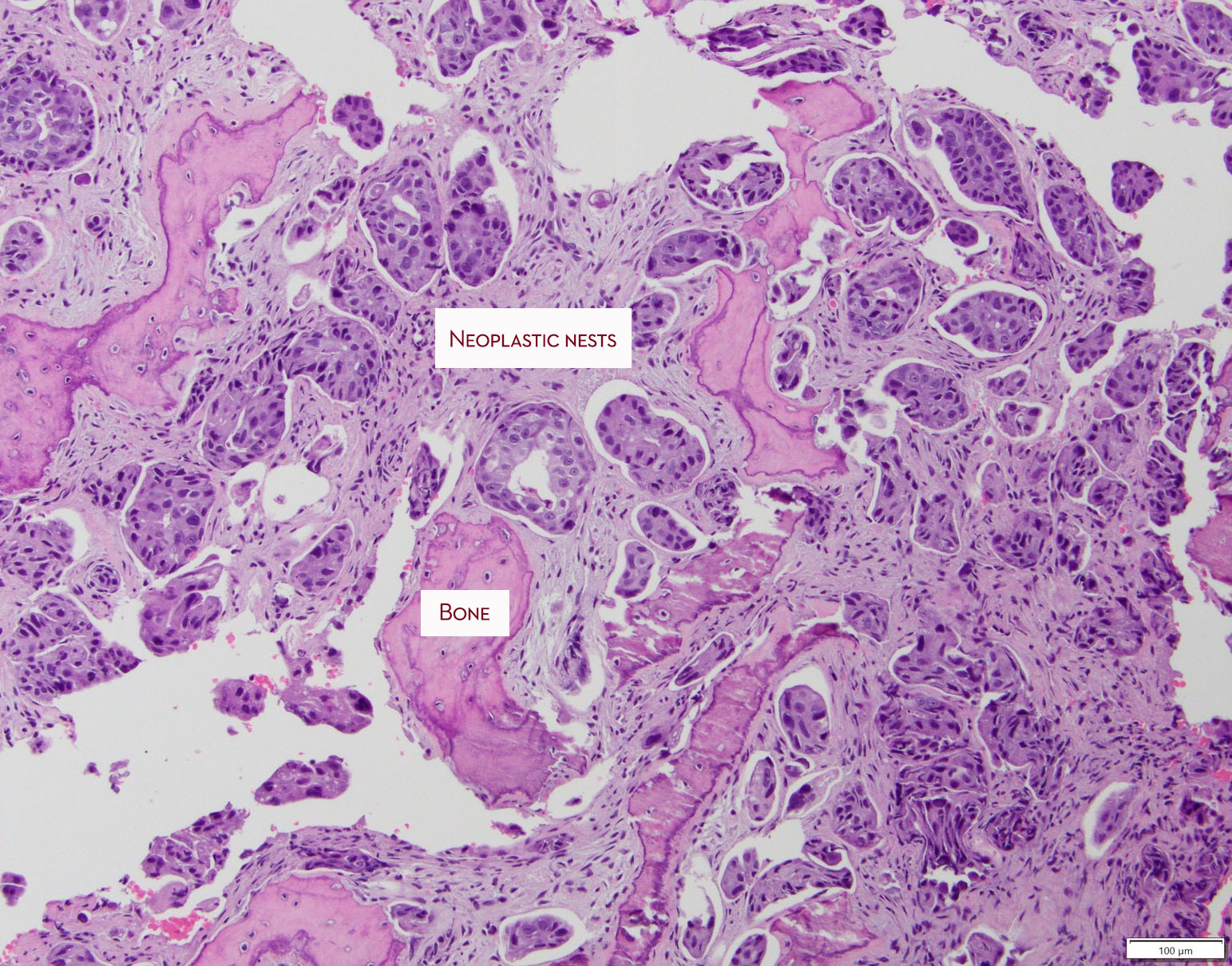
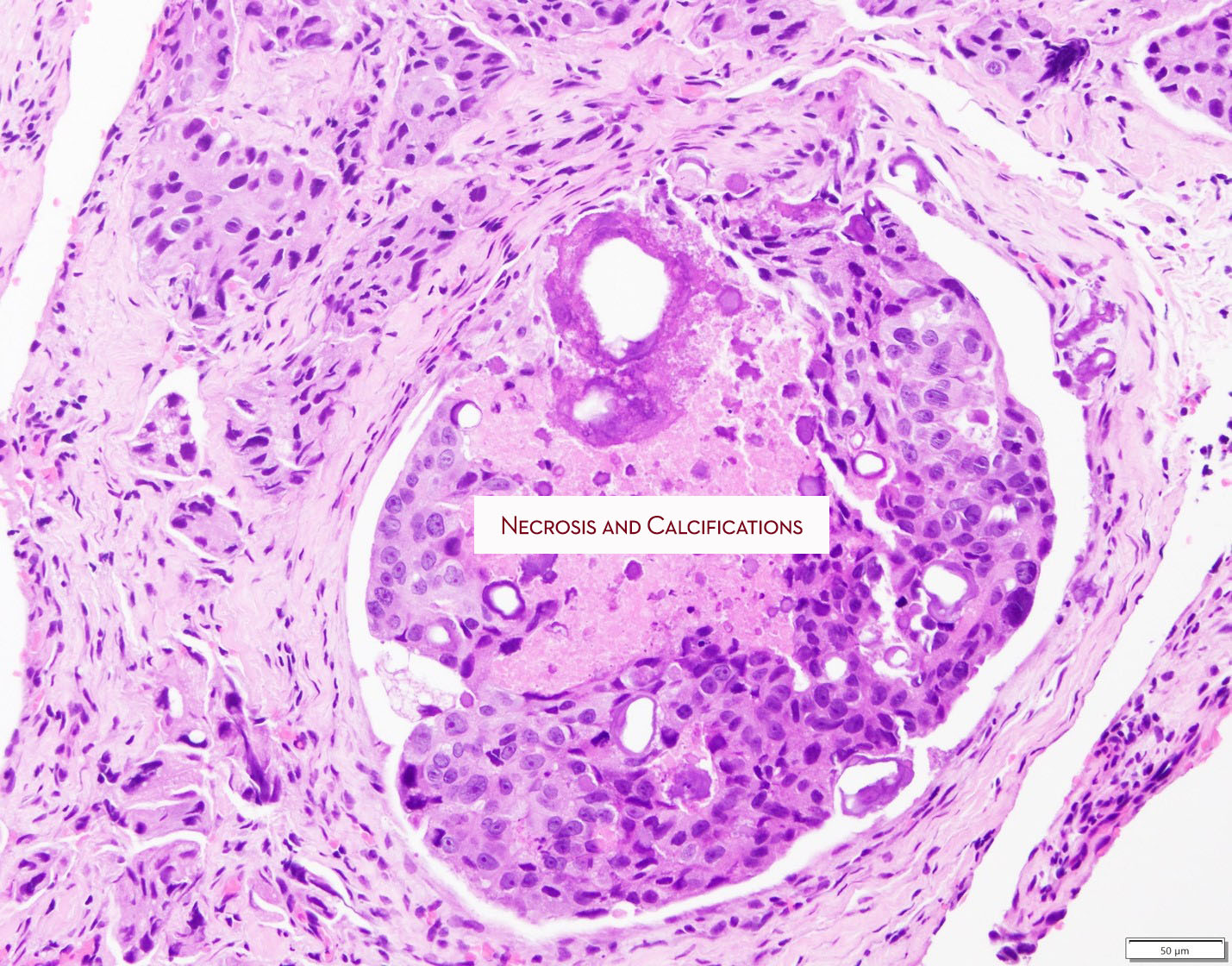
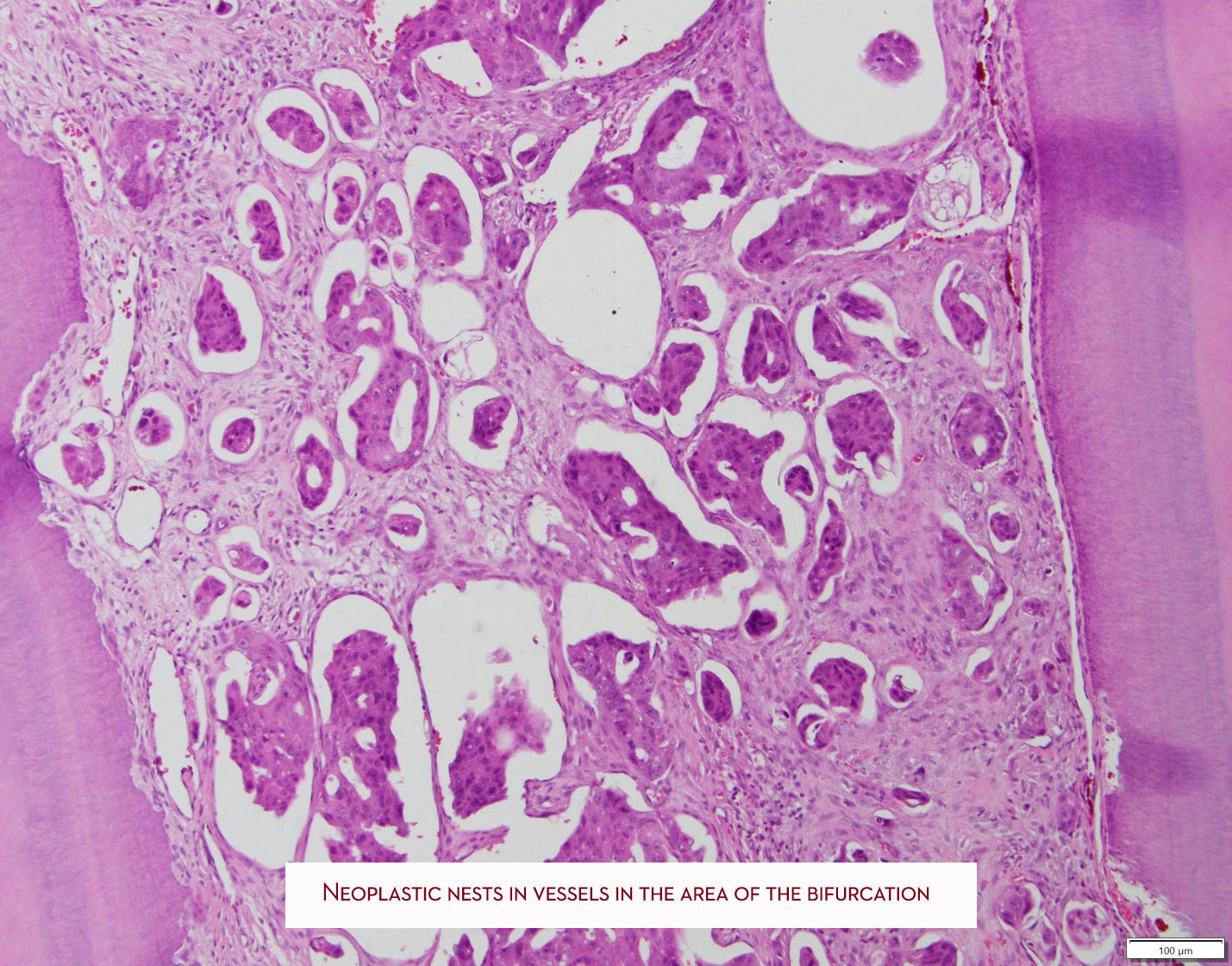
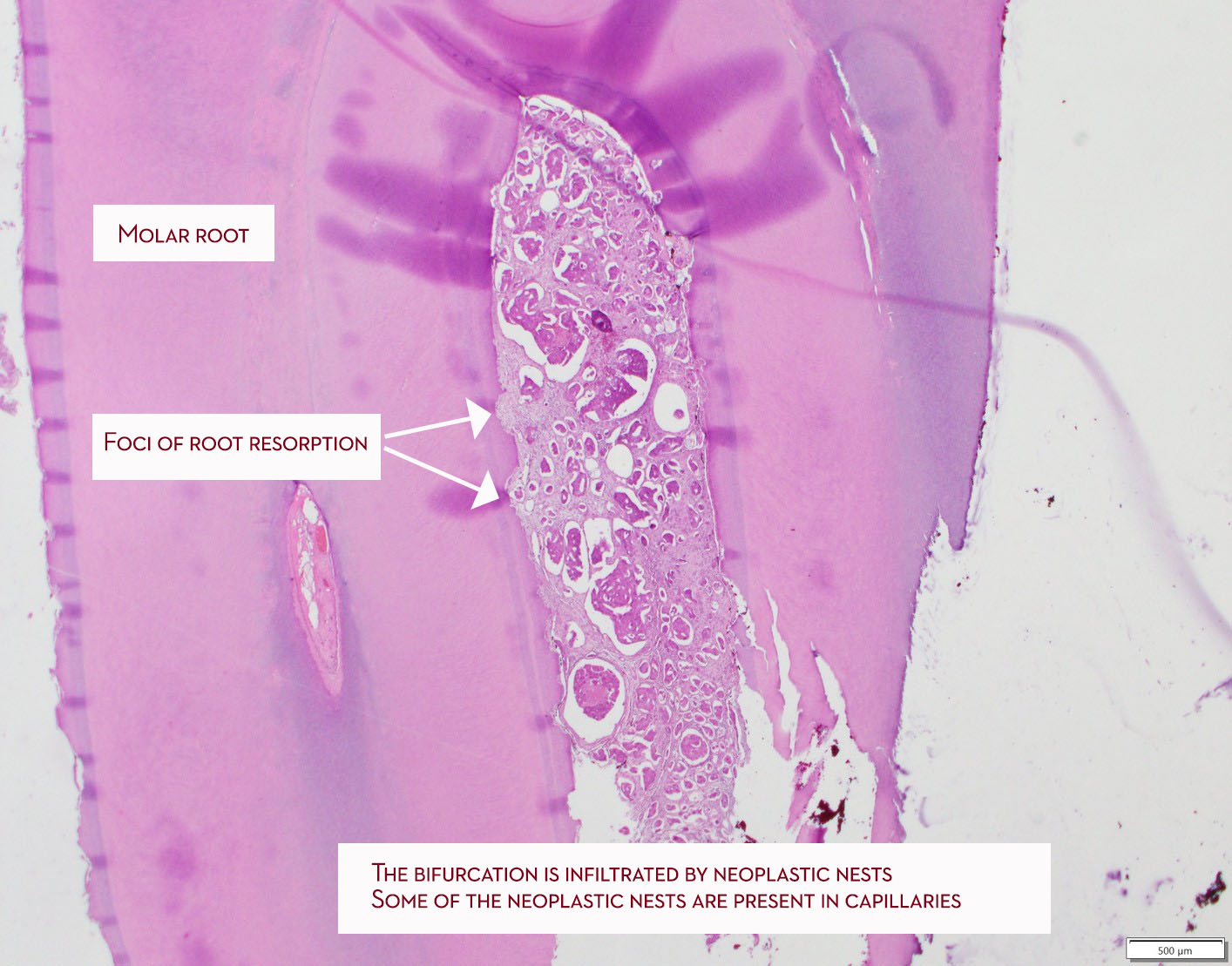
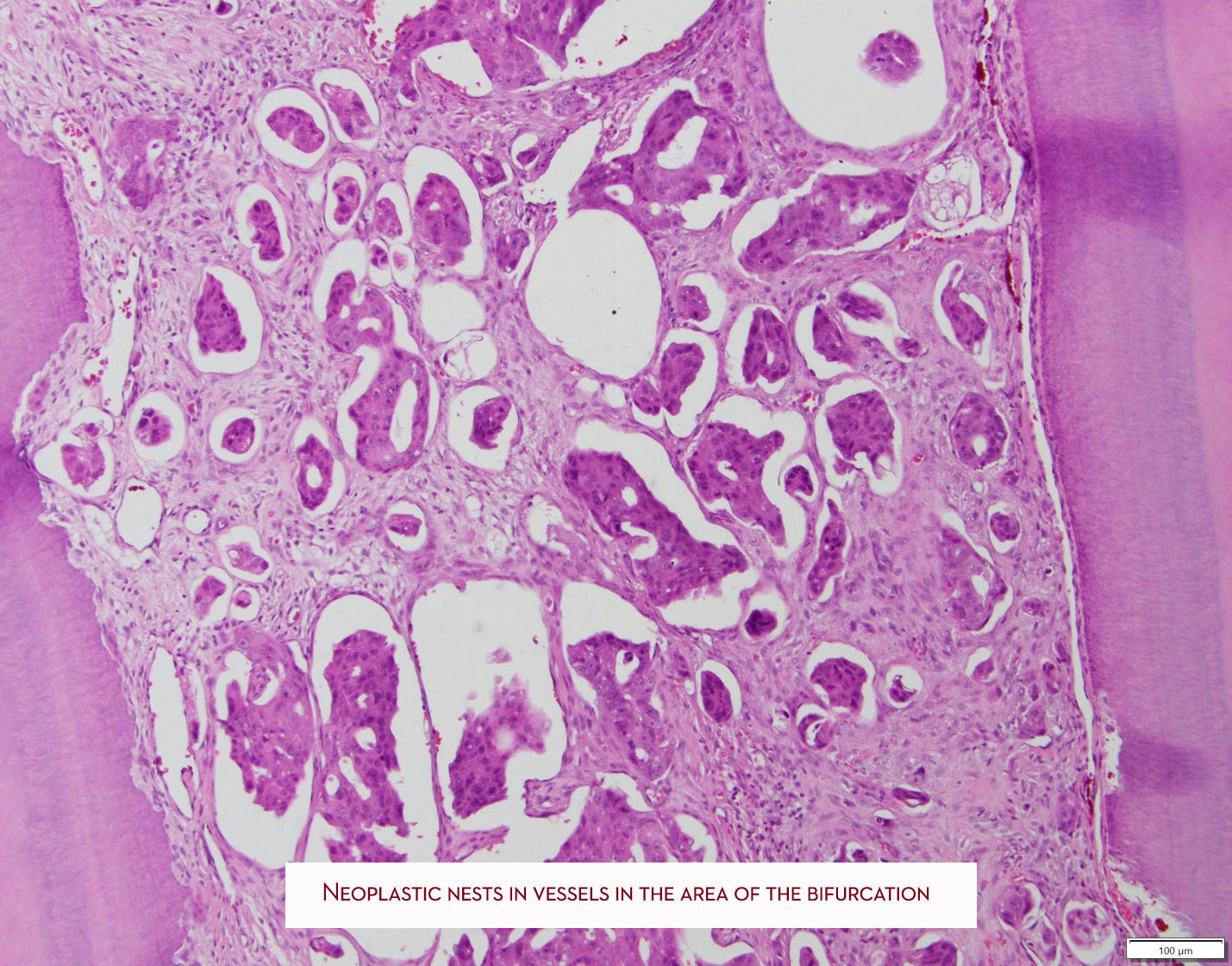
Neoplastic cells are seen in the area of bifurcation and have induced resorption of the cementum. Neoplastic nests are found in the capillaries.
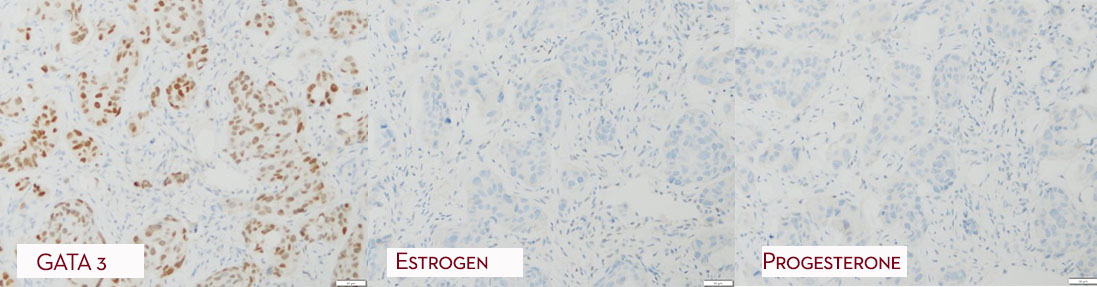
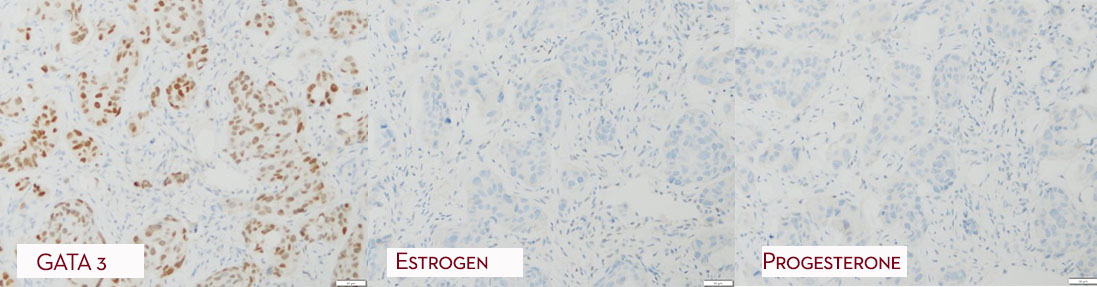
Special immunohistochemistry (GATA 3) supported the diagnosis of metastatic ductal carcinoma of the breast. The neoplastic nests were negative for estrogen and progesterone receptors and the tumor was HER2 positive.
Diagnosis
Metastatic carcinoma, breast primary, consistent with ductal carcinoma, micropapillary variant
Treatment
Such tumors with an ER/PR negative, HER2 + profile and micropapillary pattern do not have good prognosis. The patients are managed by oncologists.
Discussion
Metastatic disease to oral mucosa usually presents more frequently to the posterior mandible and presents as ill-defined, so-called moth-eaten radiolucencies. Rarely, radiopacities can be present and they reflect reactive bone formation induced by the neoplastic cells. The present tumor is unusual because it presented in the maxilla. Metastatic disease may be the first manifestation of a distant malignancy. The most frequent types of metastatic tumors to the oral soft tissues and jaws are breast, lung and colon. These patients have Stage 4 disease and, generally, their prognosis is poor.
Orthokeratinized odontogenic cyst (OOC)
Clinical Histories
1st Case
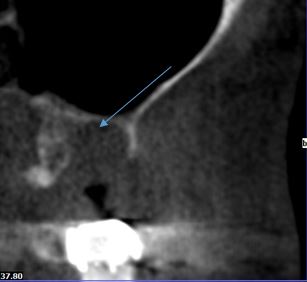
A 14 year old male presented with a unilocular radiolucency that was interfering with normal dental development. (courtesy of Dr. Dan Sampson, Oral Surgeon)
Radiographic features
Unilocular radiolucency associated with #18
Histopathologic features
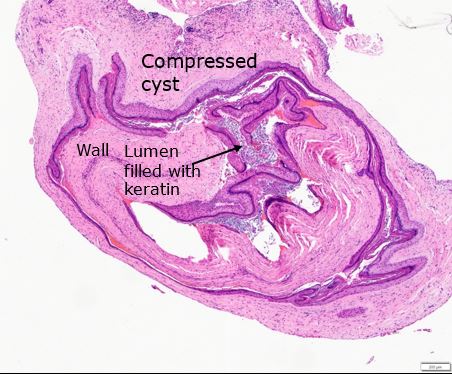
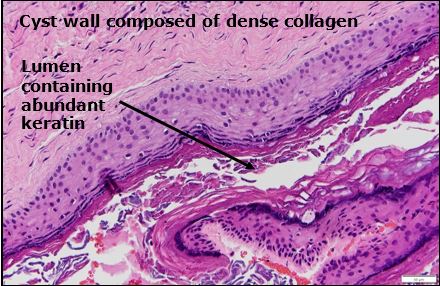
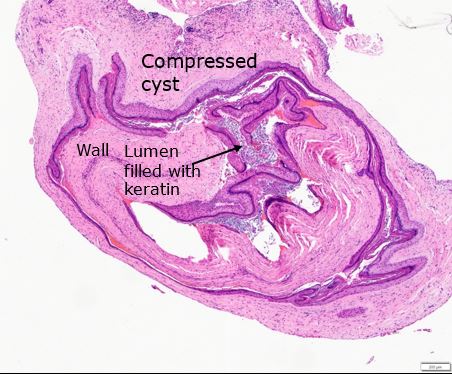
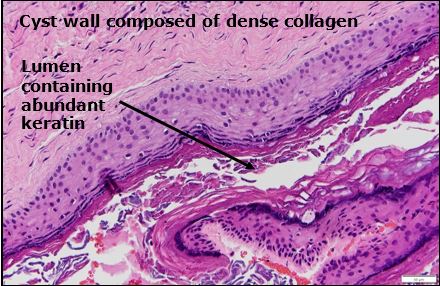
Cystic lesion was lined by thin hyperkeratinizing stratified squamous epithelium. There was no evidence of nuclear palisading and hyperchromatism in the basal cell layer. The lumen contained abundant keratin. The wall was composed of dense collagen and inflammation was unremarkable.
Diagnosis
Orthokeratinized Cyst
Treatment
Surgical enucleation
2nd Case
A 73 year old male presented with a unilocular radiolucency in the area of teeth #14 and 15. (courtesy of Dr. Brett Voegele, Oral Surgeon)
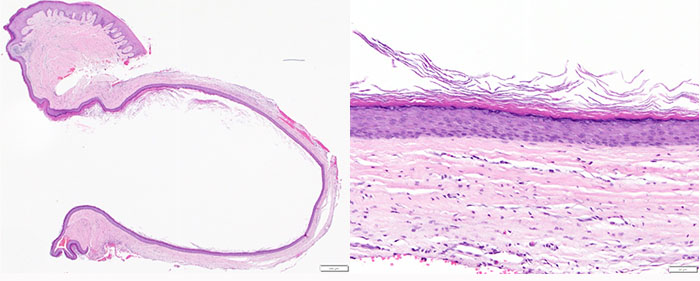
Histopathologic features
This cystic lesion was lined by thin hyperkeratinizing stratified squamous epithelium. There was no evidence of nuclear palisading and hyperchromatism in the basal cell layer. The lumen contained keratin. The wall was composed of dense collagen and inflammation was unremarkable. Interestingly, this cyst had direct connection to the surface epithelium.
Discussion
The designation of an odontogenic cyst as orthokeratinized is reserved for those jaw cysts characterized by orthokeratinized odontogenic epithelium, partially or in total. In the past, these lesions were classified as odontogenic keratocysts, orthokeratinized type. However they are definitely different, clinicopathologically, from keratocystic odontogenic tumor (KOT; aka odontogenic keratocyst).
They account for about 1% of all odontogenic cysts, the mandible is by far more frequently affected, and they are more common in males. Importantly, their recurrence rate is less than 2% according to studies, compared to KOT 30% recurrence rate.
They may be noticed as an incidental finding and they can be associated with impacted teeth. Differentiating them from dentigerous cysts at the radiographic level is impossible. Generally, they present as unilocular radiolucencies while a multilocular pattern is uncommon. Histologically, the epithelium is hyperkeratinizing with a distinct granular cell layer and no evidence of palisading and hyperchromatism in the basal cell layer and also without a corrugated surface. Keratin production can be seen in both KOT and OOC. Generally, there is no evidence of inflammation in the supporting wall and, if present, it is focal. Occasionally, radicular cysts and dentigerous cysts may exhibit foci of keratinized epithelial lining but this is only focal.
Case #2 is of interest because the cyst lining was connected to the surface epithelium. It is possible in this case that, after extraction, surface epithelium was entrapped in the healing socket and underwent proliferation and cystic changes similar to epidermal inclusion cyst. Alternatively, this cyst may have occupied an area close to the surface and its lining connected to the oral mucosal epithelium.
Palisaded encapsulated neuroma
Clinical History
62-year old male presented with 4 mm painless nodule on the hard palate in the area of the right premolars. (Clinical photograph courtesy of Dr. Troy Alton, Oral Surgeon)

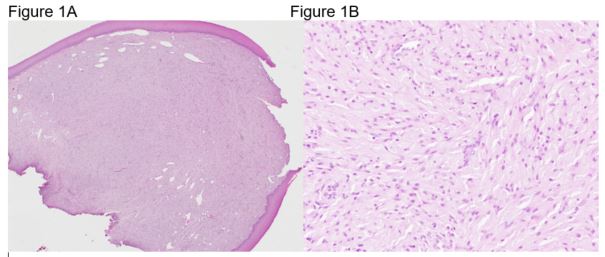
Histopathologic features
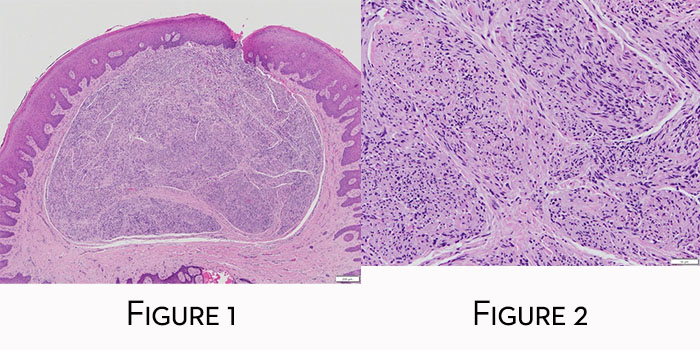
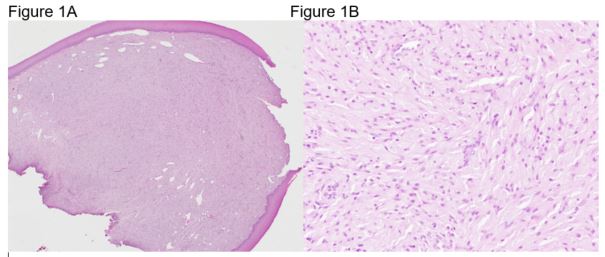
Mucosal nodule features well-delineated but unencapsulated peripheral nerve lesion (Figure 1) characterized by intermingling fascicles of Schwann cells in a fibrocollagenous stroma (Figure 2) exhibiting shrinkage or tissue retraction artifact. A delicate perineurium partially surrounds the proliferating fascicles.
Diagnosis
Palisaded encapsulated (solitary circumscribed) neuroma
Treatment
Excisional biopsy.
Discussion
Palisaded encapsulated neuroma is an uncommon oral lesion, however, it is frequent among oral peripheral nerve sheath tumors. It appears in the literature under two names, palisaded encapsulated neuroma or solitary circumscribed neuroma. Prior to its description as a separate entity, these lesions were categorized either as neurofibromas, schwannomas or traumatic neuromas. Palisaded encapsulated neuromas are only partially encapsulated and palisading is present in the minority of lesions. Thus, the term solitary circumscribed neuroma. However, even this term is not precise because there are reports of multiple confluent lesions. These lesions are described on the skin which is the most common location with the oral mucosa second in frequency.
The vast majority of palisaded encapsulated (solitary circumscribed) neuromas involves the masticatory (palate and gingiva) mucosa followed by the labial mucosa, the tongue and buccal mucosa. Extraorally, the perilabial skin is a frequent location. The histopathologic diagnosis is in the vast majority of cases simple and can be supported by immunohistochemical stains that highlight the presence of Schwann cells, nerve axons, which are plenty, and a partial perineurial envelop.
Lesions are most frequently painless, except if traumatized. Treatment is excisional biopsy and recurrence rate less than 1% according to our study.
Adenomatoid odontogenic tumor
Clinical History
15-year-old female presented with radiolucent lesion between the lower permanent canine and first premolar with slight expansion of the mandible. The differential diagnosis provided included keratocystic odontogenic tumor (odontogenic keratocyst), ameloblastoma and lateral periodontal cyst (Contributor: Dr. Luke MacMenamin, Oral Surgeon).
Radiographic features
Panoramic radiograph reveals unilocular radiolucency with root divergence (Figure 1). The lesion extended, apparently, through the buccal cortex (Figure 2).
Histopathologic features
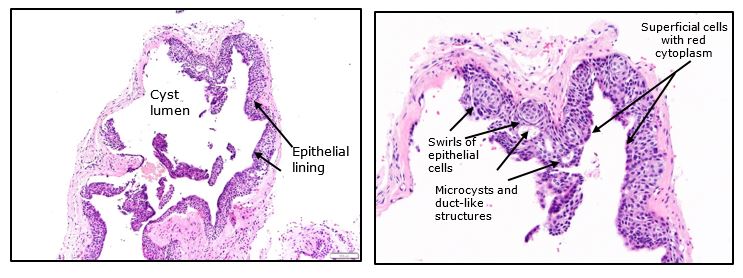
Low power microscopy reveals cystic lesion with odontogenic epithelial proliferation into the lumen and along the epithelial lining and formation of small nodules with duct-like structures, rosettes and whorls (Figure 1). Higher power of a representative area reveals whorls of epithelial cells and duct-like structures (Figure 2)
Diagnosis
Adenomatoid odontogenic tumor
Treatment
The lesion was enucleated. No recurrence has been reported.
Discussion
Adenomatoid odontogenic tumor (AOT) is a benign epithelial odontogenic tumor accounting less than 5% of all odontogenic tumors. It occurs, more frequently, in the anterior maxilla. The maxilla is twice more frequently affected than the mandible with strong predilection of the anterior aspect of the jaws. Females are twice more frequently affected than males with 75% of cases occurring in teenagers. Three quarters of the cases are associated with an impacted tooth. Patients are usually asymptomatic and mild expansion may be observed, however, cortical perforation is unusual. Rare extra-osseous examples have been described in the literature.
Radiographically, the lesions are unilocular radiolucencies. Radiopacities may be seen in some cases and are generally small. They represent dystrophic calcifications occasionally present in the tumors. Displacement of teeth and root divergence can be observed; however, root resorption is rare.
A FACTOID TO REMEMBER
The classic presentation of AOT is as a radiolucent or mixed radiolucent/opaque lesion of the anterior maxilla in a teenage girl with impacted canine. A radiographic clue when dealing with an impacted tooth is that the radiolucency in AOT usually starts below the CE junction.
Histopathologically, the lesions are characterized by solid or cystic pattern where one identifies nests exhibiting whorls and rosettes, as well as duct-like structures. The latter finding gives the tumor an adenoid appearance, thus the designation adenomatoid. In the past the tumor was referred to as adenoameloblastoma, however, this term has been abandoned and we discourage its use.
The treatment of choice is enucleation. Recurrence is exceedingly rare.
Herpes Simplex
Clinical History
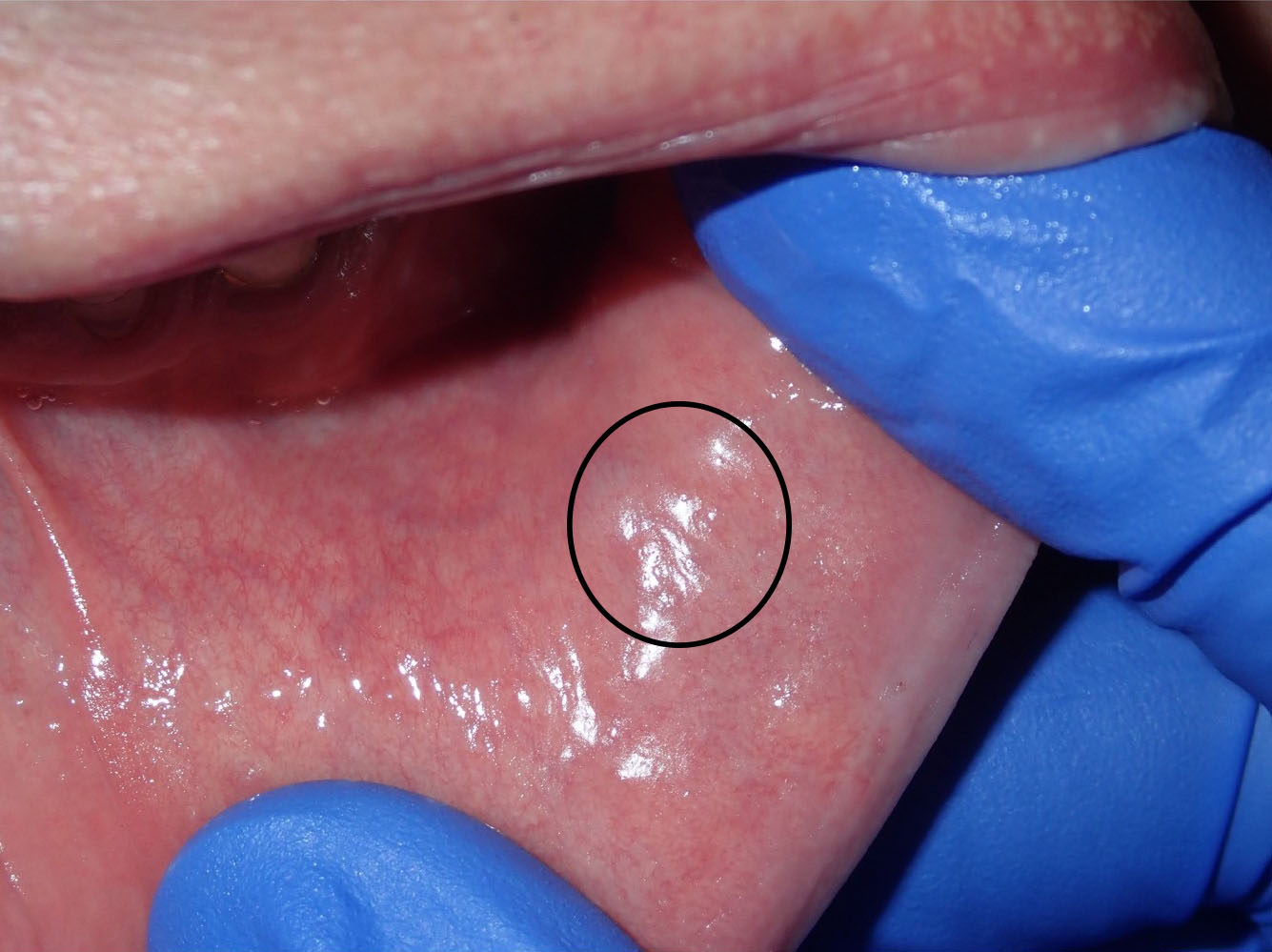
An 80-year-old male presented with multiple ulcers with surrounding erythema preceded by vesicles that coalesced. The patient has polymyalgia rheumatica and had, recently, a flare-up. He was treated by prednisone. (clinical photograph courtesy of Dr. James Block, Oral Surgeon).
Clinical features
Ulcer covered by pseudomembrane with erythematous halo. Smaller erosions or ulcers anteriorly

Histopathologic features
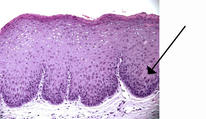
The mucosal fragment was ulcerated and featured so-called cytopathic effect in individual epithelial cells which is related to herpetic infection. Viral inclusion bodies were present in the nuclei of epithelial cells. Immunohistochemistry confirmed the presence of herpes simplex virus infection of the surface epithelium.
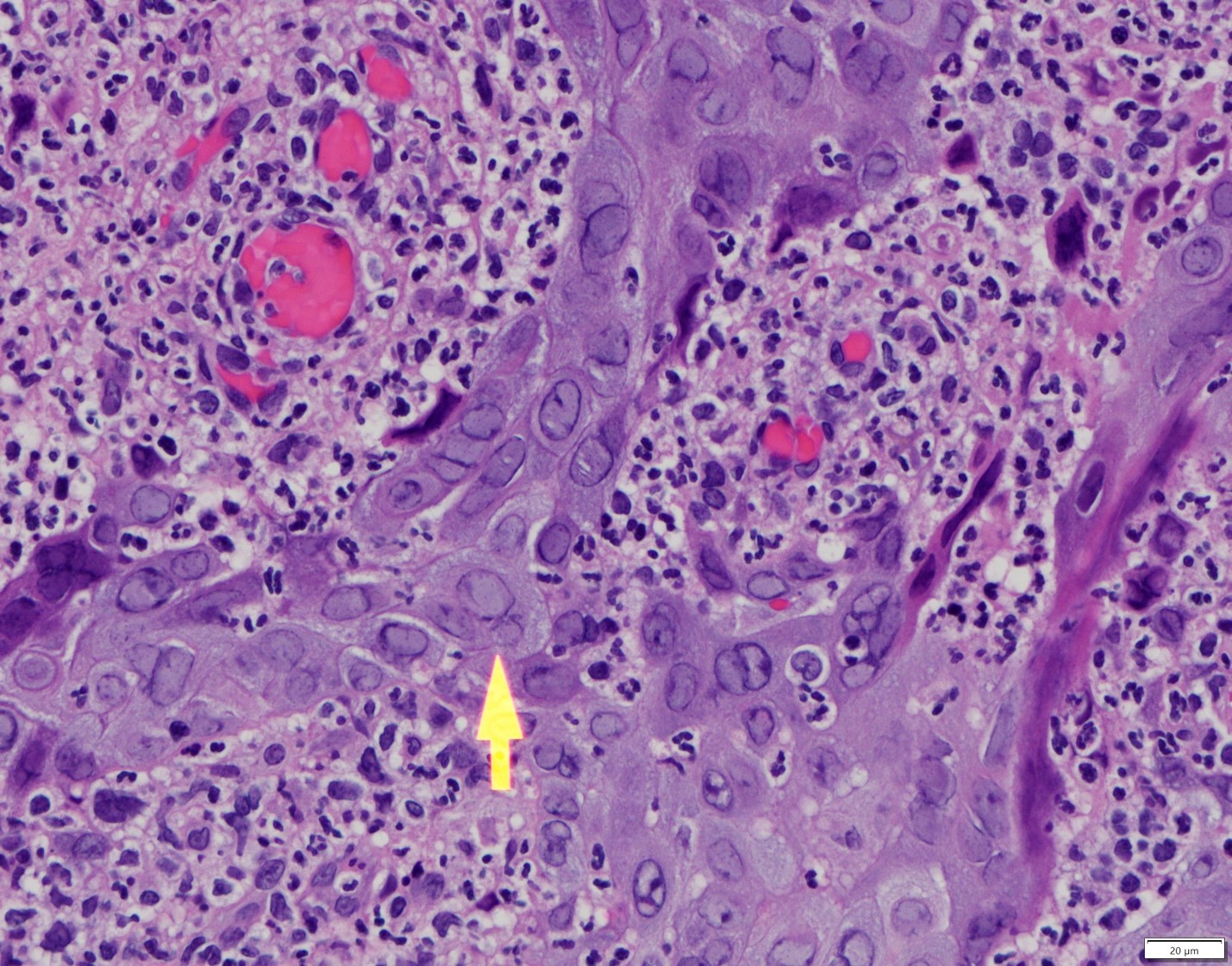
The arrow points to epithelial cells infected by herpes virus. The nucleus is enlarged and has a ground-glass appearance. Other cells feature magenta color nuclei.
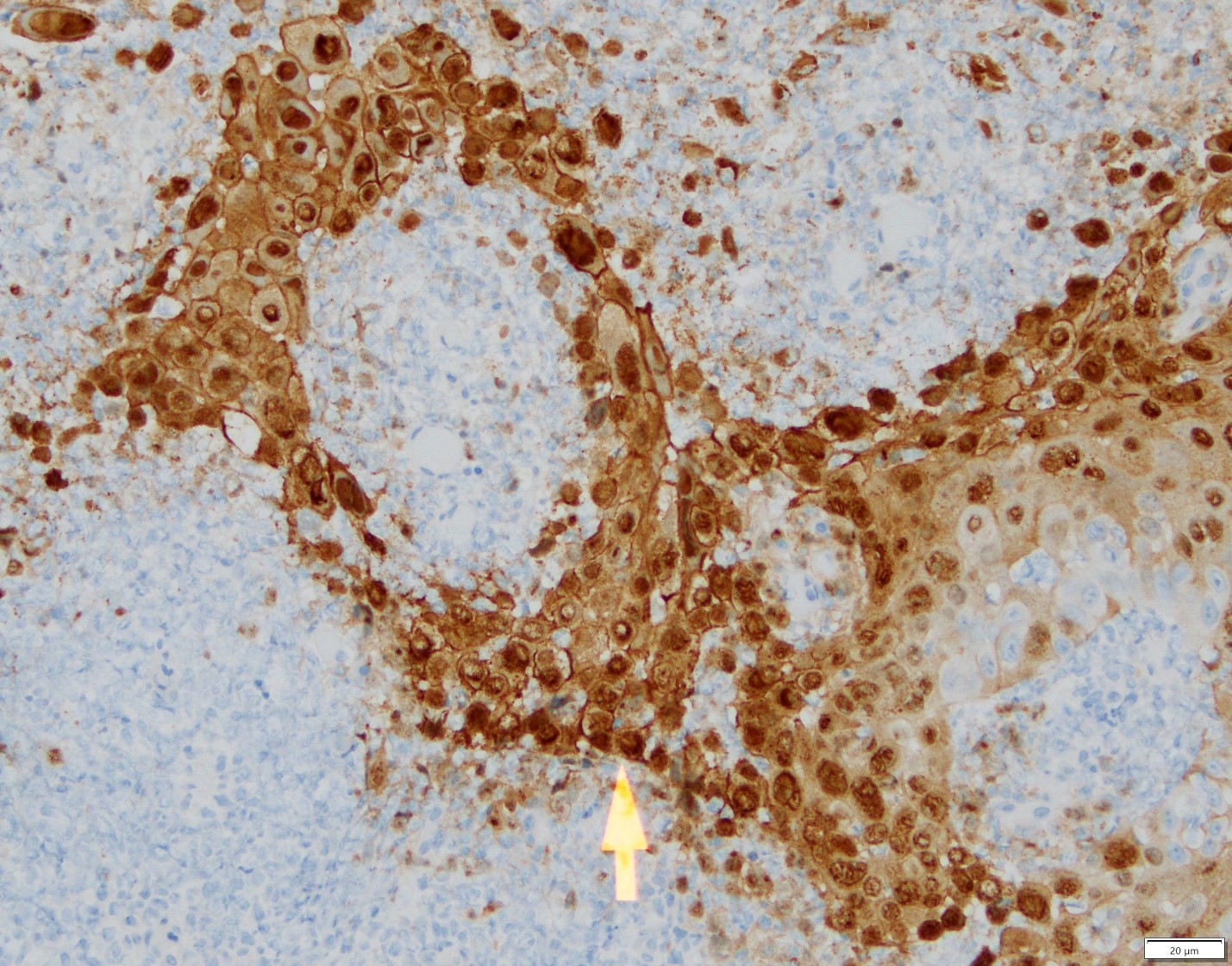
Immunohistochemical evaluation confirmed the presence to herpes simplex virus in individual epithelial cells.
Diagnosis
Ulcer with herpes simplex virus (HSV) cytopathic effect
Treatment
For older patients and patients with recurrent herpes, valacyclovir or famciclovir demonstrate effectiveness and the dosing is convenient for the patients. In patients who present with active lesions such as the case above, tapering off or discontinuation of the immunosuppressive medication may lead to faster resolution of lesions. Certainly, valacyclovir or famciclovir can be used to probably accelerating the healing process. Interestingly, a combination of oral valacyclovir 2 g orally twice daily and clobetasole gel 0.05% twice daily for 3 days can reduce the mean maximum lesion size and mean healing time of classical lesions*.
Discussion
In this particular example, old age and treatment with prednisone can be triggering factors for herpetic infection by herpes simplex virus.
*Hull C, McKeough M, Sebastian K, Kriesel J, Spruance S. Valacyclovir and topical clobetasol gel for the episodic treatment of herpes labialis: a patient-initiated, double-blind, placebo-controlled pilot trial. J Eur Acad Dermatol Venereol. 2009 Mar;23(3):263-7.
Mucoepidermoid carcinoma
Clinical History
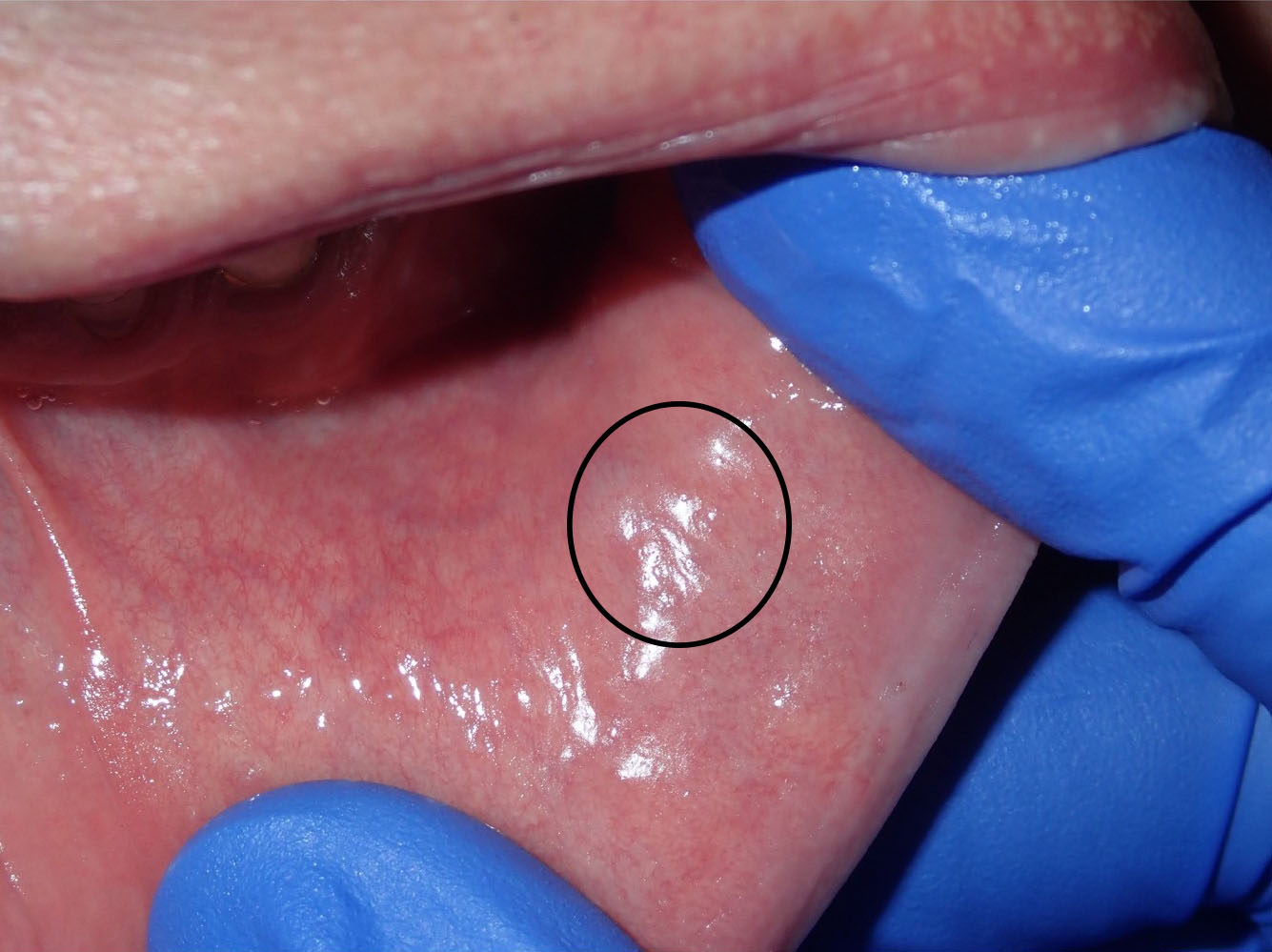
A 66-year-old male presented with a firm, mobile lesion on the inner surface of the lower lip opposite to teeth #23 and 24, that was slightly compressible and measuring 0.5x0.5 cm (clinical photograph courtesy of Dr. Nick Spanel, Oral Surgeon).
Histopathologic features
Histopathologic preparation revealed cystic lesion featuring two cavities lined by ductal, squamoid (epidermoid) and, in foci, mucous cells. Mild cytologic variations without mitotic activity were observed. In addition and in deeper sections, predominantly, rare nests of mucous, optically clear and squamoid cells were evident.
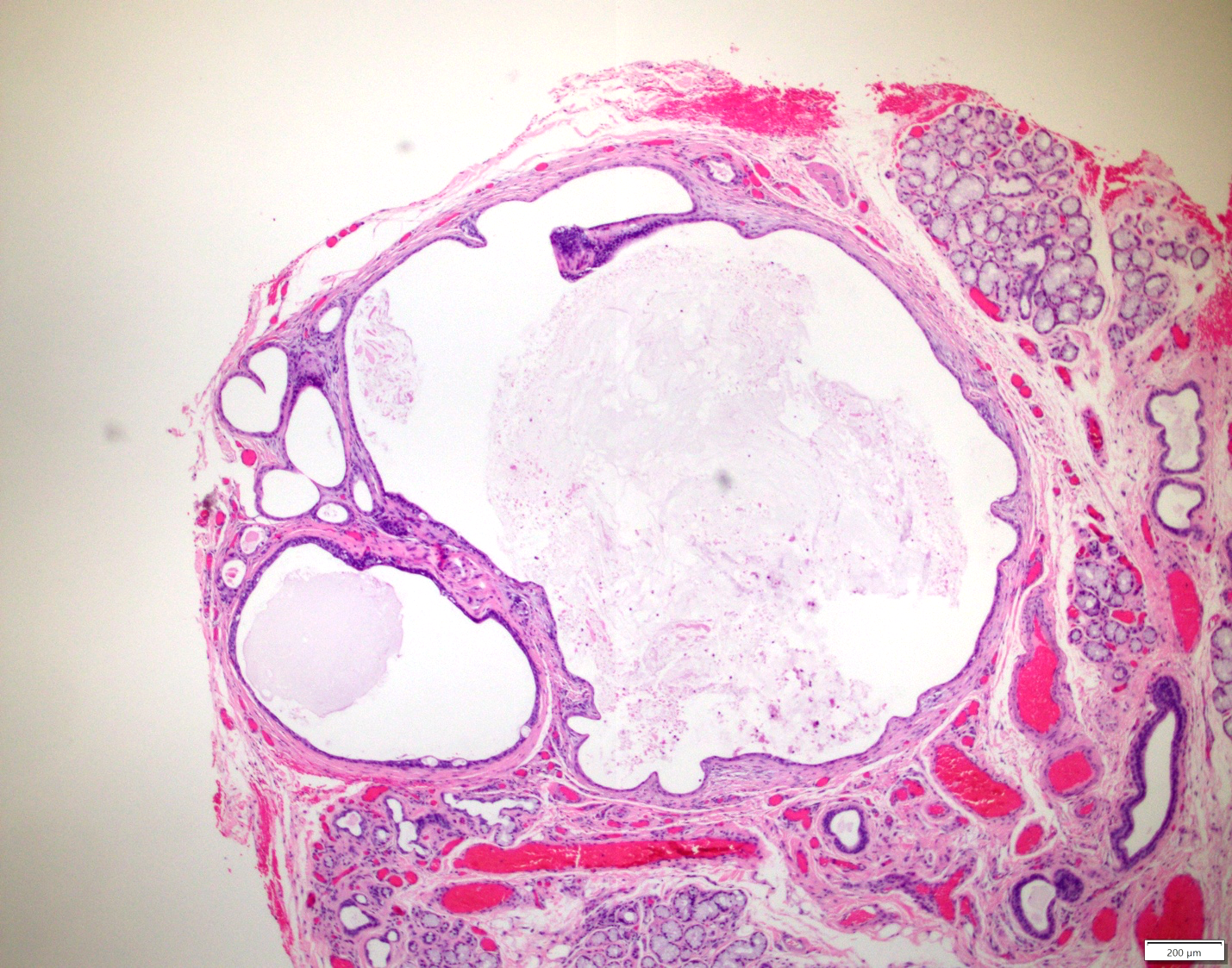
The greatest dimension of the tumor was measured at 2.2 mm. Cavities of various sizes were lined by neoplastic cells.

Diagnosis
Mucoepidermoid carcinoma
Treatment
Excision with tumor free margins is indicated for intraoral tumors. Most frequently intraoral tumors are low-grade and do not metastasize. In the present example, the tumor was contained within the surgical specimen. The patient will be followed.
Discussion
This is one of the smallest examples of mucoepidermoid carcinoma observed in our laboratory. Mucoepidermoid carcinoma is the most frequent malignant salivary glands tumor of major and minor salivary glands. The most frequent location for intraoral mucoepidermoid carcinoma is the posterior hard palate and the soft palate. The lower lip is an uncommon site. The clinical differential diagnosis, given the patient’s age should include salivary gland neoplasia. If trauma is excluded, as a rule, an older individual with a cystic lesion in the lower lip, does NOT have an extravasation type mucocele until proven otherwise. Mucoceles in older individuals are most frequently of the retention type and are seen more frequently in the upper lip.
In the present case, the cells of the neoplastic nests harbored aberrations of a gene known as MAML2. This gene is frequently rearranged in mucoepidermoid carcinomas but not in other malignant salivary gland tumors.
Oral Leukoplakia - Low-grade dysplasia
Clinical History
A 40-year-old male presented with the lesion on the right ventrolateral border of the tongue. The patient is a 15 pack-year smoker. The clinical picture is courtesy of Dr. Troy Alton, Oral Surgeon, Madison, WI.

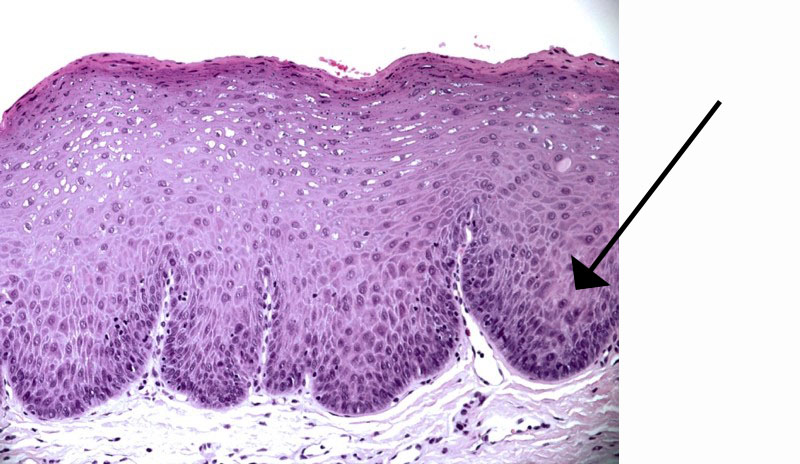
Histopathologic features
Mucosal fragment was surfaced by hyperparakeratinizing and acanthotic stratified squamous epithelium exhibiting cytologic and architectural variations consistent with low-grade (mild) premalignant epithelial dysplasia.
Basal cell hyperplasia with nuclear hyperchromatism and perturbed stratification of the cells. The thickening of the epithelium makes the color of the lesion look white. The changes are present in the lower part of the epithelium and there are few. However, these changes justify the designation low-grade premalignant epithelial dysplasia.
Discussion
Clinically, the lesion has the characteristics of so-called oral leukoplakia, an oral potentially malignant disorder. According to the World Health Organization, in western countries, the prevalence of leukoplakia generally ranges from 1-4%. Many cases of leukoplakia are associated with tobacco use with or without heavy alcohol consumption. However, some are not and among them few may be related to high risk human papilloma virus (HPV) infection.
Oral leukoplakia is a clinical term used to describe white variations in the oral mucosa that cannot be clinically classified as any other entity. Generally, leukoplakic lesions should be biopsied to evaluate the histologic characteristics of the lesion. Many times leukoplakic lesions are histologically characterized only by epithelial tissue hyperplasia. For the case above, an incisional biopsy was taken and the histology revealed mild (low risk) epithelial dysplasia. Cytologic variations that were interpreted as dysplasia were evident in the lower one third of the surface epithelium.
Sometimes the white plaques of leukoplakia are associated with red (erythematous) areas. In such case the term erythroleukoplakia is used. The presence of a clinical erythematous component increases the possibility of histologic dysplastic changes in the surface epithelium.
In our case after the histopathologic diagnosis was communicated to the clinician, the entire lesion was excised and evaluated for dysplasia-free margins. Interestingly, in the excised specimen, the lesion revealed foci of moderate (high risk) dysplasia in addition to the residual mild dysplasia. The patient is placed on follow-up. Follow-up is important because recurrence may occur and, in some patients, new lesions may arise in other areas.
These lesions include leukoplakia and erythroleukoplakia, the lateral being more frequently associated with dysplasia at the microscopic level.
The interpretation of dysplasia relies on the identification of the following architectural and cytologic abnormal variations
| Architectural | Cytologic |
| Perturbed stratification | Nuclear size |
| Loss of polarity in the basal cell layer | Nuclear shape |
| Mitotic activity in suprabasal areas | Cell size |
| Increased number of mitoses | Cell shape |
| Dyskeratosis; premature keratinization | Nuclear/cytoplasmic ratio |
| Keratin pearls within rete ridges | Atypical mitoses |
| Acantholysis | Increased number and size of nucleoi |
| Abnormal rete ridges; drop-shaped, club-shaped; interconnected, etc... | Nuclear hyperchromatism |
Two different grading systems exist to grade dysplasia. In one, the dysplasia is graded as mild, moderate or severe. The other grading system is binary; low risk and high risk dysplasia, the latter lumping moderate and severe grades. After discussions and review of many histopathologic examples of dysplasia we have decided to use the binary system and this will be implemented this August.
The cut-off point between mild (low-risk) and moderate-severe (high risk) is if four or more architectural and four or more cytologic variations from the list above are observed.
Management of oral premalignant epithelial dysplasia
We suggest the following algorithm when dealing with patients with oral potentially malignant disorder.
Clinical Assessment of the Lesion
- Photography
- Incisional or excisional biopsy
Histopathologic diagnostic possibilities
- Low risk (mild) dysplasia or just epithelial hyperplasia
- If there is clinical concern (non-homogeneous lesion*, lesion size >200 mm2, tongue/floor of mouth location, patient is a smoker, presence of an erythematous component) à resection by a specialist (scalpel or laser); close monitoring of the patient (e.g. one month after the procedure, then every 3 months for the first year, every 6 months the second year and then yearly for at least 5 years to life) by a specialist, i.e. oral surgeon; clinical photography is highly recommended at every appointment..*Rebiopsy may be indicated in cases of non-homogeneous lesions
- If there is no clinical concern (see above) --> monitoring (every 4-6 months) or resection followed by monitoring as above.
- High risk (moderate or severe dysplasia)
- Resection by a specialist and monitoring as above.
Below are two excellent references on the subject of management of oral dysplasia.
- Awadallah M, Idle M, Patel K, and Kademani D. Management update of potentially premalignant oral epithelial lesions. Oral Surg Oral Med Oral Pathol Endo. 2018 Jun;125(6):628-636.
- Field EA, McCarthy CE, Ho MW, Rajlawat BP, Holt D, Rogers SN, Triantafyllou A, Field JK, Shaw RJ. Oral Oncol 2015;51:883-887.
EBV-positive mucocutaneous ulcer
Clinical history
A 64-year old male presented with an ulcerated lesion in the posterior right retromolar mucosa. The patient had heart transplantation. (Clinical photograph courtesy of Dr. Karl Andreasen, Oral Surgeon)

Histopathologic features
Ulcerated lesion revealed proliferation of atypical lymphoid cells harboring Epstein-Barr virus encoding RNA and exhibiting positivity for lymphoid markers CD15 and CD30. The inflammatory population was characterized by B and T cells.
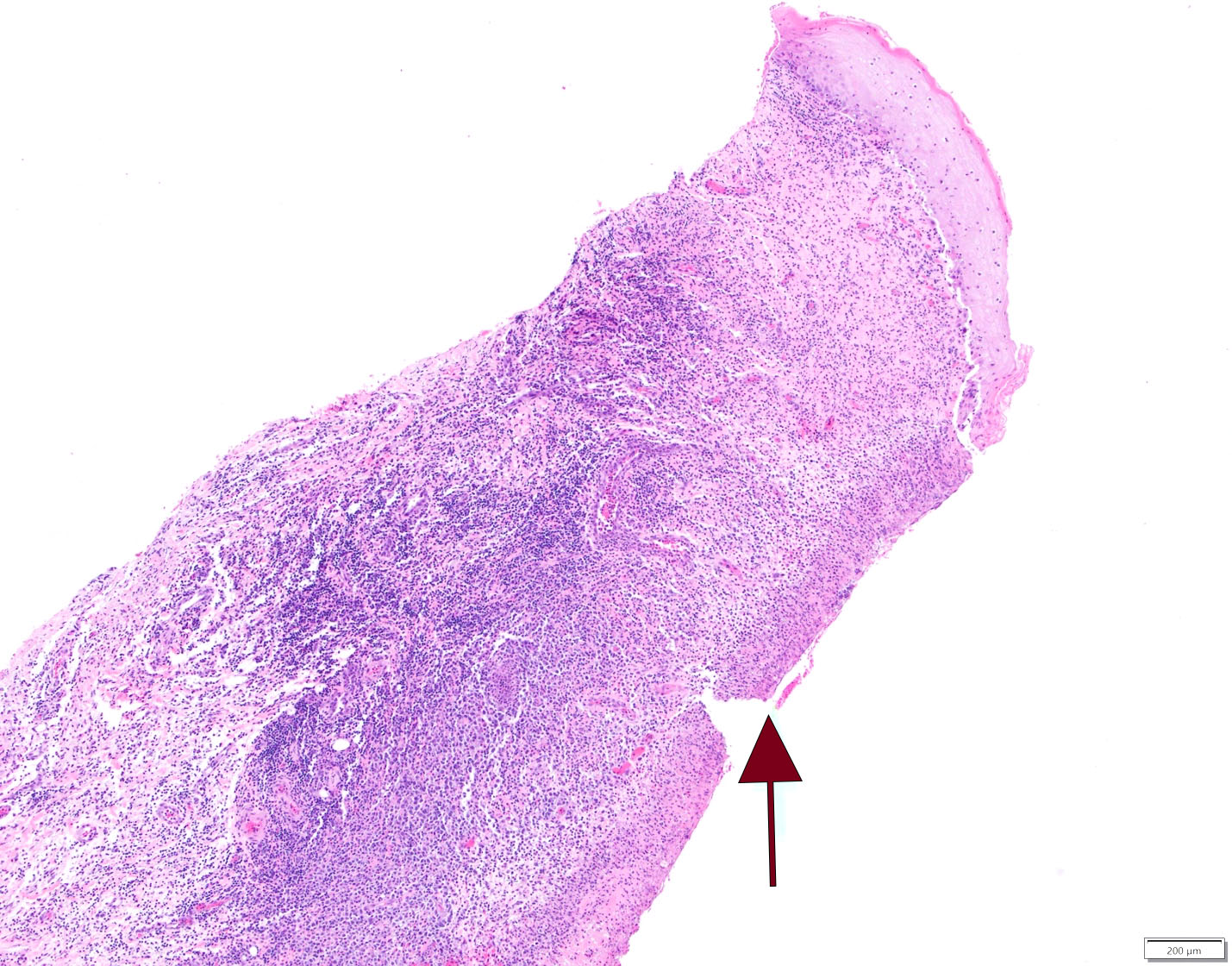
This is an ulcer. The arrow points to the ulcerated surface. At the upper right corner there is a residual surface epithelium.
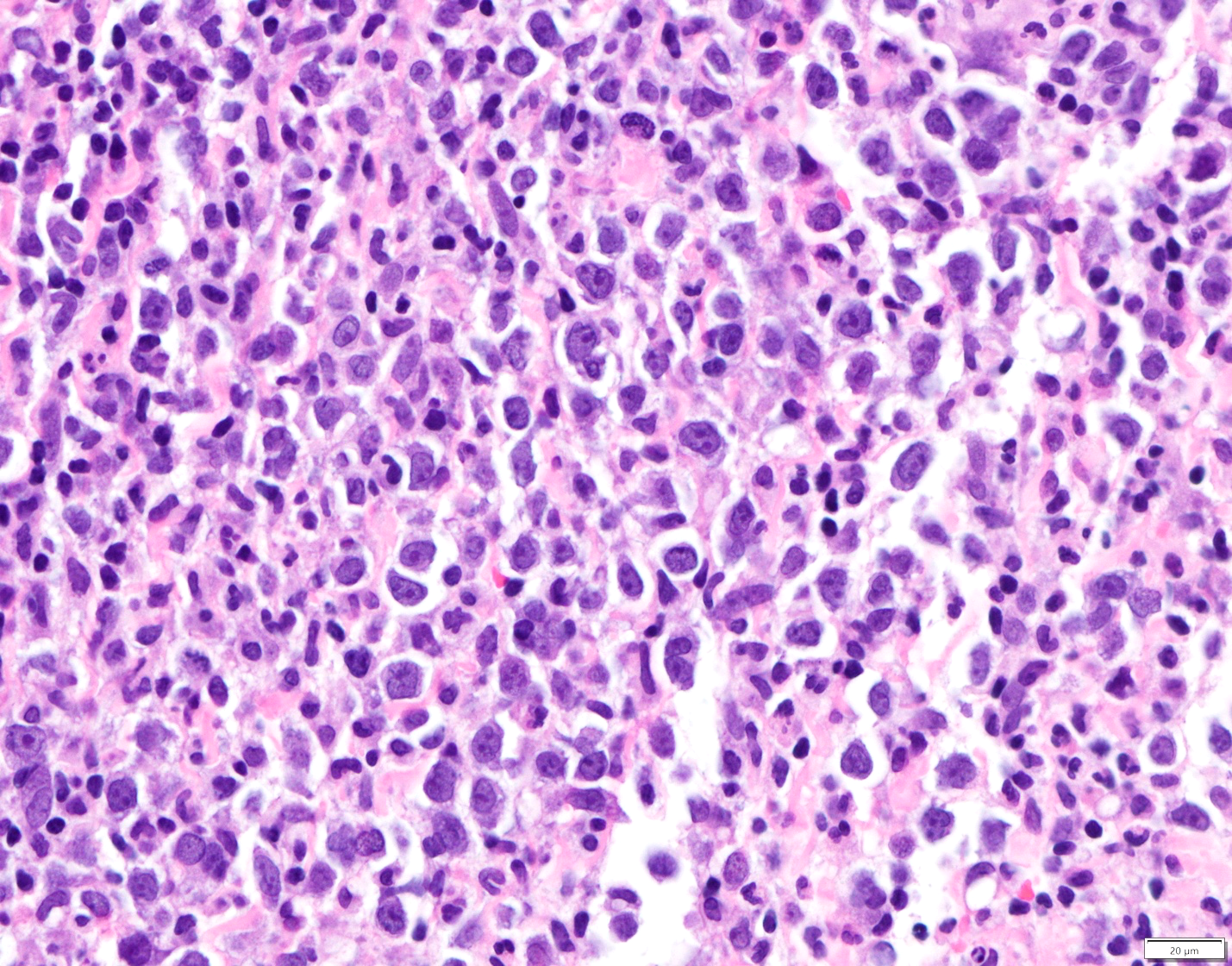
Atypical lymphoid cells are present in this infiltrate characterized by B and T lymphocytes.

In situ hybridization reaction on the tissue highlights with purple cells harboring Epstein-Barr encoding RNA.
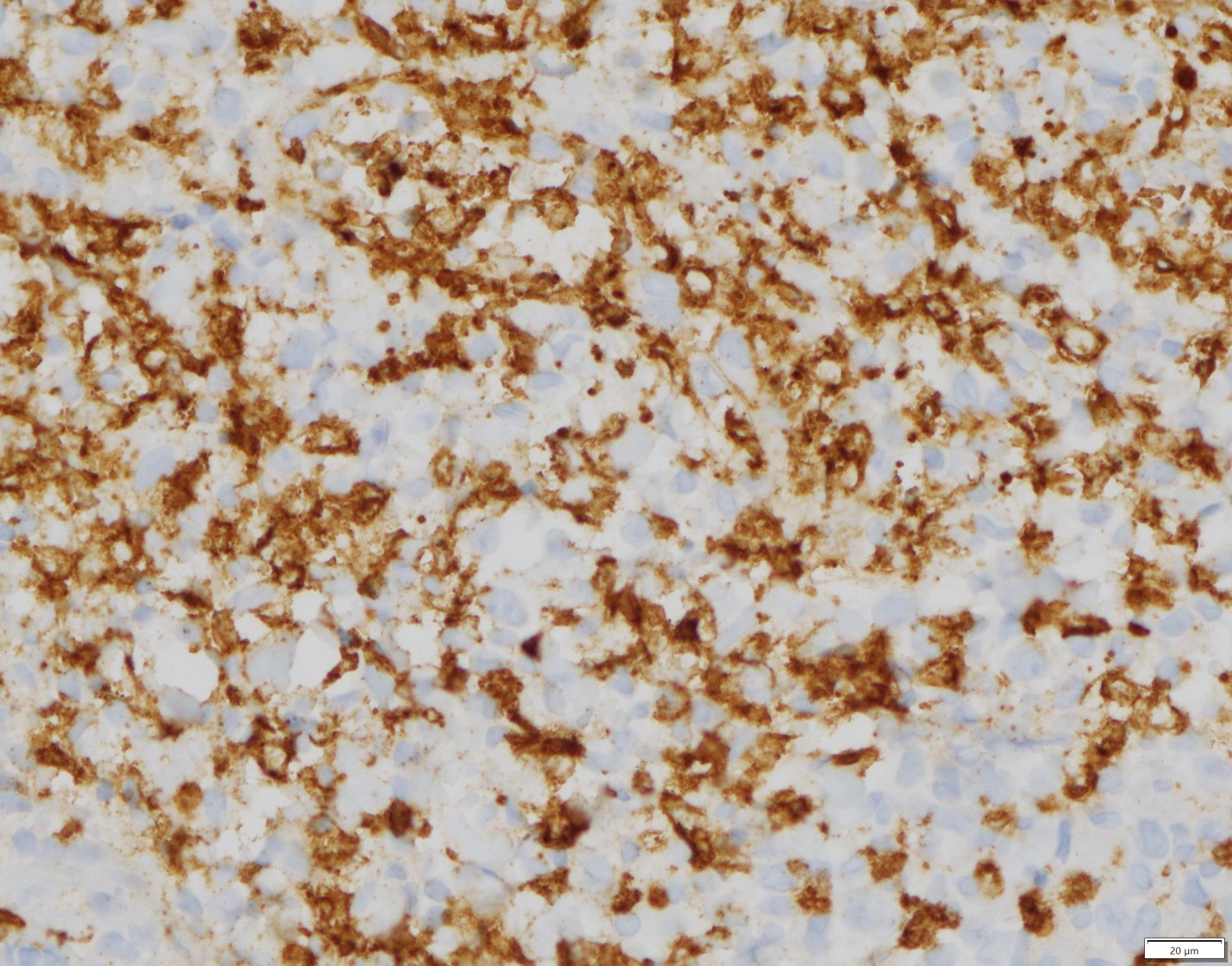
An immunohistochemical stain highlights atypical lymphoid cells exhibiting CD15 positive reaction. CD15 positivity is present in Hodgkin’s lymphoma. However, EBV mucocutaneous ulcers feature also CD15 positive cells.
An immunohistochemical stain highlights atypical lymphoid cells exhibiting CD30 positive reaction. CD30 positivity is present in anaplastic lymphomas and Hodgkin’s lymphoma. However, EBV mucocutaneous ulcers feature also CD30 positive cells.
Diagnosis
EBV-positive mucocutaneous ulcer
Treatment
EBV-positive mucocutaneous ulcer may be the result of advanced age and immunosenescence. Referral to a physician is recommended. For cases in which medication-related immunosuppression is the culprit, the patient should be referred back to his oncologist or transplant surgeon as it was the case with the patient described herein.
If the patient is on immunosuppressive medication, reduction of the dose may lead to complete healing. Those patients for who reduction is not indicated, are treated with monoclonal antibody agents such as rituximab, radiation or other chemotherapeutic agents. A few patients may develop widespread disease or some other form of EBV-positive lymphoproliferative disorder (see below) including lymphoma.
Discussion
Iatrogenic immunosuppression has lead to the development of new pathologic processes affecting occasionally the oral mucosa. One such example is EBV-positive mucocutaneous ulcer. The name implies that these lesions may develop on the skin or mucosal sites including the oral cavity. In many cases EBV-positive mucocutaneous ulcer is related to advanced age. Immunosuppressive medications such as methotrexate, azathioprine, cyclosporine or tumor necrotic factor inhibitors have also been reported as driving factors for the development of such ulcers.
Clinically, oral ulcers may be painful and look aggressive with the clinical differential diagnosis including squamous cell carcinoma. The lesions are many times seen in areas prone to trauma. Besides the mouth and the skin, lesions have been described in the intestinal mucosa.
Oral pathologists are expected to be familiar with these lesions. Careful evaluation of the inflammatory infiltrate and identification of large cells transformed by EBV in association in the presence of intense inflammation can lead to the proper diagnosis which is further confirmed by immunohistochemical stains and in situ hybridization for EBV-encoding RNA. Some cases can resemble lymphoma and sometimes the distinction is very difficult. Also, some cases can look like Hodgkin’s lymphoma (disease) but such neoplasm is very rare in the oral mucosa.
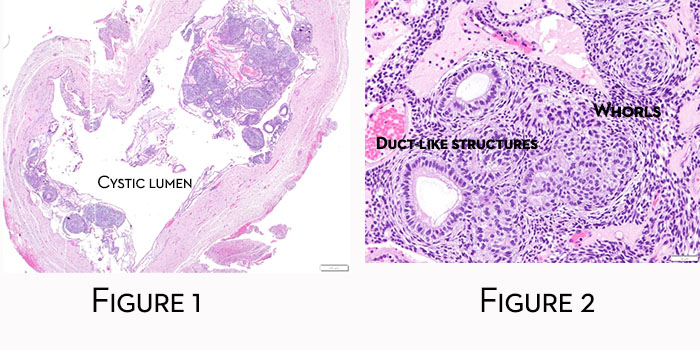
Glandular Odontogenic Cyst
Clinical History
A 54 year old male presented with buccal swelling apical to #27, 28 and pain of 3 months duration. The patient has a history of root canal treatment of teeth #27-29. Aspiration of the lesion revealed transudate. On surgical exposure of the site; thin cystic lining was noted. The cystic lesion was excised and cystic contents were mainly transudate and cheese-like material. The surrounding bone was noted to be intact. Tooth #27 had grade 1 mobility. The clinical differential diagnosis was ameloblastoma or radicular cyst (Courtesy of Drs. Aarathi Rao and Robert Nadeau, Oral Surgery resident and Oral Surgeon, respectively)
Radiographic features
Multicameral radiolucency of the anterior mandible
Histopathologic features
Cystic lesion was lined by by thin epithelium with foci of thicker plaques of epithelial cells, occasionally featuring swirls, and cells with cytoplasmic clearing. Cuboidal cells with deep eosinophilic (red) cytoplasmic staining or low-columnar cells were also identified facing the lumen. Mucous cells were also present. The lining included various numbers of microcysts or duct-like structures.
Diagnosis
Glandular odontogenic cyst (GOC)
Treatment
Treatment is usually enucleation but recurrences are frequent. If the patient is compliant; repeated enucleation may be indicated. However, large and multilocular lesions, especially with history of recurrence, may be treated with en bloc resection.
Discussion
GOCs are rare developmental odontogenic cysts accounting for less than 1% of all odontogenic cysts. They are more frequently encountered in middle-aged adults. Radiographically, GOCs present as unilocular or multilocular radiolucencies. The most common site is the anterior mandible with lesions crossing the midline. This is contrast to ameloblastomas which can also be multilocular, but are more frequently encountered in the posterior aspect of the mandible.
Close follow-up is expected in all patients with GOCs given a recurrence rate of 30-50%. Occasionally, dentigerous cysts may exhibit foci reminiscent of GOC. Association of GOC with impacted teeth is uncommon. Be that as it may, a comment is provided with the diagnosis of dentigerous cyst when features reminiscent of GOC are noticed to alert the clinician of the diagnostic possibility of a possible developing GOC.
Microscopically, the cystic lining of the glandular odontogenic cyst is characterized by thin epithelium with foci of thicker plaques of stratified squamous epithelium, occasionally featuring swirls, and cells with cytoplasmic clearing. Cuboidal cells with deep eosinophilic (red) cytoplasmic staining or low-columnar cells are are identified facing the lumen. Mucous cells are also present. The lining includes also various numbers of microcysts or duct-like structures. Papillary projections into the lumen can be also seen.
Histologic features of GOC can in some cases be indistinguishable from mucoepidermoid carcinoma, especially when nests of odontogenic epithelium with features of mucoepidermoid carcinoma are noticed in the connective tissue lining. There is ongoing debate about mucoepidermoid carcinoma arising in the lining of glandular odontogenic cysts or if some cysts diagnosed as GOC are in fact mucoepidermoid carcinomas. For such cases, a comment usually accompanies the pathology report and close follow-up of the patient is indicated.
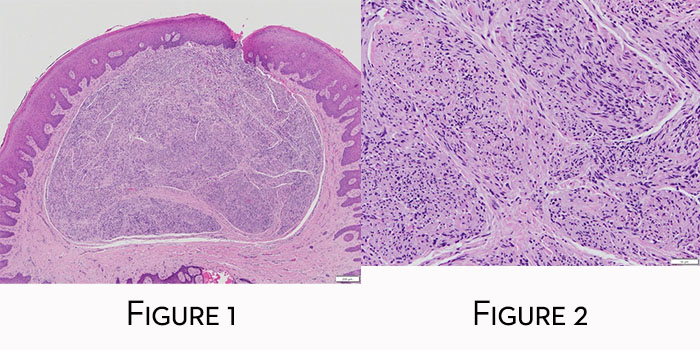
Osteosarcoma
Clinical History
A 20 y/o female, who is 24 weeks pregnant, presented for evaluation of right submandibular and sublingual swelling along with V3 paresthesia associated with partially erupted #32. A 4-month old panoramic radiograph showed no overt radiolucency (Figure 1). The third molar was extracted for presumed pericoronitis. Upon extraction of the tooth significant abnormal tissue was noted apical and mesial to #32 area. A new panoramic radiograph was taken (Figure 2) which reveals moth eaten bone in right mandible and root resorption associated with #31. An incisional biopsy was taken with the lesions being suspicious for osteomyelitis versus osteosarcoma (Courtesy of Dr. Tyler Varhol, Oral Surgeon)
Radiographic features
The radiograph in Figure 1 features partially erupted right third mandibular molar. Subtle radiopacity is present on the distal aspect of the mesial root of tooth #31.
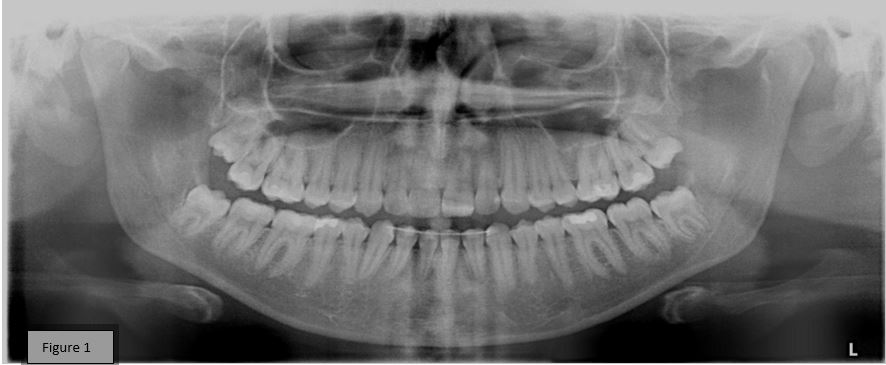
Figure 2 reveals larger radiopacity on the distal aspect of the mesial root of tooth #31 with associated root resorption, as well as mixed lucent and opaque variations in association with tooth #32 and extending proximally to tooth #30 and distally to tooth #31.

Histopathologic features
Incisional biopsy revealed proliferation of sheets (Figure 3) of predominantly spindle cells exhibiting spindle or ovoid hyperchromatic nuclei and spindle cytoplasm (Figures 4&5). Individual cells featured pleomorphism and mitoses. These neoplastic cells formed osteoid (Figure 4&5) with foci of calcifications (Figure 5). The stroma was characterized by increased vascularity. A special immunohistochemical stain, SATB2 (Figure 6), a transcriptional regulation and chromatin remodeling DNA binding protein, decorated neoplastic cells.
Diagnosis
Osteoblastic osteosarcoma
Discussion
Osteosarcoma of the jaws is a rare form of sarcoma. There are three major types of osteosarcoma and all three can affect the jaws. These types are central, surface and extraskeletal. Central osteosarcoma is the most common of the three and has three major subtypes, osteoblastic, chondroblastic and fibroblastic. There are some rarer forms also, i.e. telangiectatic, small cell, osteoblastoma-like, etc. The surface or juxtacortical type has three subtypes, parosteal, periosteal and high-grade surface. The present type is central osteoblastic.
Radicular cyst and CGCL
Clinical History
A 73-year old male presented on 01/19/2019 for routine dental care when a draining lesion was noted on clinical examination in the maxilla (Courtesy of Dr. Brett Moore, Plymouth MN).
Radiographic features
The lesion was traced to the apex of tooth #10 which was associated with a radiolucent lesion (Figure 1A). The tooth was non-responsive to cold. Root canal treatment was completed on 1/23/2019 (Figure 1B). The patient went back to clinic in July 2019 with radiolucency appearing to heal but the sinus tract still present. The patient was referred to an endodontist but did not pursue the referral. The patient returned to clinic on 1/22/2020 with persistent sinus tract. He was given the option to go to an endodontist for evaluation or to amputate root to preserve the bridge with removal of cyst and grafting. The patient decided the latter and the surgical procedure was completed on 2/26/2020.
Histopathologic features
The specimen revealed an inflamed odontogenic cyst lined by non-keratinizing thin stratified squamous epithelium. In the wall of the cyst another process was present which was characterized by multiple fibroblasts and multinucleated giant cells in a hemorrhagic stroma.
Diagnosis
Central giant cell lesion and radicular cyst
Treatment
Excision with follow-up of the patient
Discussion
While radicular cyst is the most common odontogenic cyst of the jaws, central giant cell lesions are uncommon. Rarely, a giant cell lesion may be seen in association with another lesion in jaws, e.g. odontogenic cyst or odontogenic tumor like ameloblastoma. In the present case we cannot determine which came first, the cyst or the giant cell lesion. Regardless, the patient should be followed because giant cell lesions can recur. Another name that is issued for central giant cell lesion is central giant cell granuloma. When the diagnosis of central giant cell lesion is made, it is prudent to refer the patient to their physician for laboratory evaluation of calcium, phosphate and parathormone levels. Although in most instances central giant cell lesions are solitary without an underlying systemic cause, the possibility of hyperparathyroidism cannot be excluded by means of histopathology and radiology alone.
Congenital epulis
Clinical History
A 15-day-old female with slight nursing difficulty presented with an 1 cm in greatest dimension fibrous nodular lesion on the right anterior side of the maxillary alveolar ridge (Figure 1A). The lesion was present at birth and has become somewhat bigger. The lesion was excised (Courtesy of Dr. Chelsea Erickson, East Grand Forks, MN).

Radiographic features
The bone was not involved
Histopathologic features
Nodular lesion (Figure 1A) was surfaced by non-neoplastic thin parakeratinizing stratified squamous epithelium. In the connective tissue sheets of granular cells in a rich vascular stroma were present. There were also foci of mild inflammation.
Diagnosis
Congenital epulis (congenital granular cell lesion, congenital granular cell epulis)
Treatment
The lesion was excised and recurrence is not expected.
Discussion
Congenital epulis is seen primarily in female newborns with a female to male ratio approaching 10:1. Although there is such female predilection, lesions do not harbor progesterone or estrogen receptors. Lesions present as solitary polyps with the maxillary alveolar mucosa 2-3 more frequently affected than the mandibular. The histogenesis of the lesion is unknown but the possibility of an unusual odontogenic lesion cannot be ruled out. The size of the lesions is approximately 1-2 cm but larger lesions have been described causing difficulties in breastfeeding or using a baby bottle. Surgical excision is the treatment of choice although complete regression has been described in some patients with partial excision or even without any treatment.
Arteriovenous hemangioma
Clinical History
27-year-old female presented with non-raised erythematous lesion (arrow) on the palate 0.5 cm in greatest dimension which blanched when pressed. The lesion did not affect the bone (Courtesy of: Jason Leet, Resident in Oral Surgery and Madeleine Gamble, Orthodontics Resident in Orthodontics)
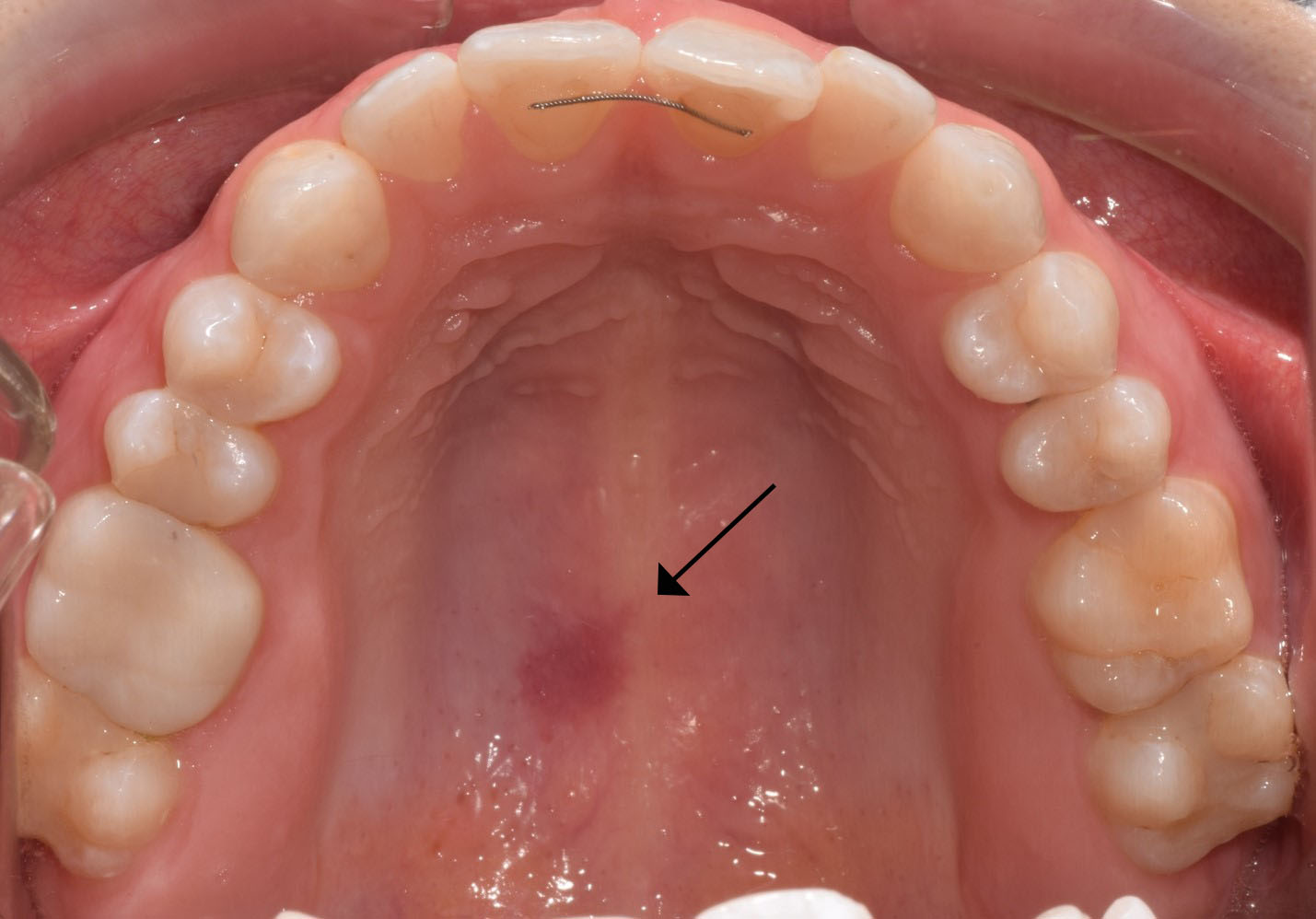
Histopathologic features
The mucosal fragment is covered by non-neoplastic keratinizing stratified squamous epithelium and reveals, in the lamina propria, multiple capillaries with occasionally conspicuous smooth muscle wall (star). These capillaries have properties of arterioles (red arrow) and venules (blue arrow). Included in the connective tissue are portions of mucous minor salivary glands (black arrow).
Diagnosis
Arteriovenous hemangioma (proliferation)
Treatment
The lesion was excised and the patient will be followed.
Discussion
Arteriovenous hemangioma (AVH) is an uncommon vascular proliferation seen on the lips, tongue, palate, gingiva and alveolar mucosa. Women are slightly more frequently affected than men. The lesions are generally small and can present either as nodules or as flat erythematous macules. In most instances, they are characterized by diffuse proliferation of capillaries with properties of arterioles and venules. The etiology is uncertain and trauma may be responsible for this vascular proliferation or malformation. Some lesions may be true hamartomas. Surgical excision is the treatment choice with approximately 11% recurrence rate.
Metastatic breast cancer to maxilla
Clinical History
A 42-year-old female with history of breast cancer presented with rapid onset of bone loss associated with teeth # 2-5 which tested vital. There was no evidence of periodontal pockets. CBCT scan showed erosion of maxillary sinus floor and root resorption associated with at least tooth # 2. (Contributed by Dr. Dan Sampson, Oral Surgeon)
Radiographic features
The tumor presented with spiked dental root resorption and tumor affecting the right sinus.
Histopathologic features
Nests of neoplastic cells of infiltrated the bone. Neoplastic cells vary in size and exhibit nuclear hyperchromatism and mitotic activity. Some of the nests feature necrosis of cells and there are dystrophic calcifications.
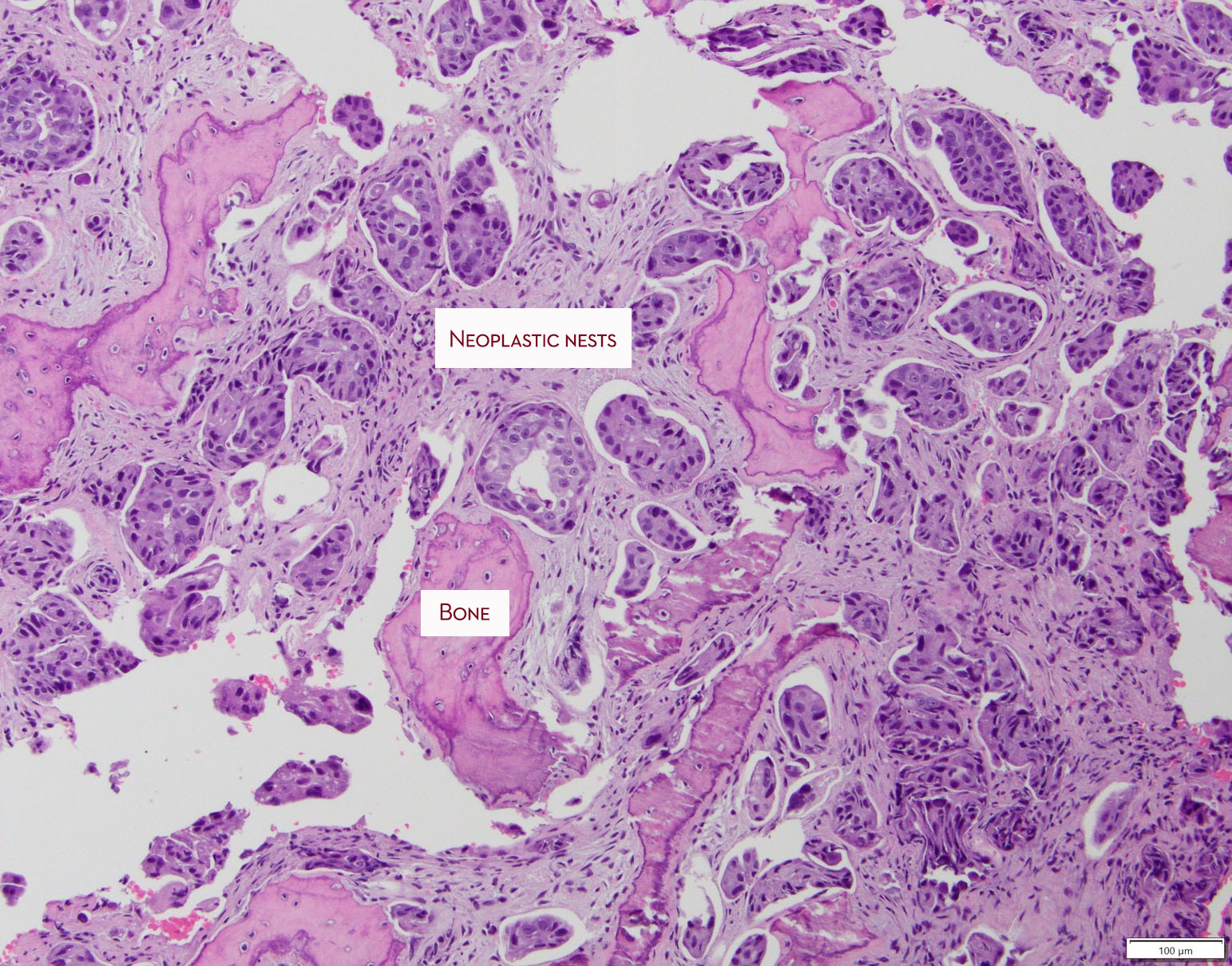
Neoplastic cells are seen in the area of bifurcation and have induced resorption of the cementum. Neoplastic nests are found in the capillaries.
Special immunohistochemistry (GATA 3) supported the diagnosis of metastatic ductal carcinoma of the breast. The neoplastic nests were negative for estrogen and progesterone receptors and the tumor was HER2 positive.
Diagnosis
Metastatic carcinoma, breast primary, consistent with ductal carcinoma, micropapillary variant
Treatment
Such tumors with an ER/PR negative, HER2 + profile and micropapillary pattern do not have good prognosis. The patients are managed by oncologists.
Discussion
Metastatic disease to oral mucosa usually presents more frequently to the posterior mandible and presents as ill-defined, so-called moth-eaten radiolucencies. Rarely, radiopacities can be present and they reflect reactive bone formation induced by the neoplastic cells. The present tumor is unusual because it presented in the maxilla. Metastatic disease may be the first manifestation of a distant malignancy. The most frequent types of metastatic tumors to the oral soft tissues and jaws are breast, lung and colon. These patients have Stage 4 disease and, generally, their prognosis is poor.
Orthokeratinized odontogenic cyst (OOC)
Clinical Histories
1st Case
A 14 year old male presented with a unilocular radiolucency that was interfering with normal dental development. (courtesy of Dr. Dan Sampson, Oral Surgeon)
Radiographic features
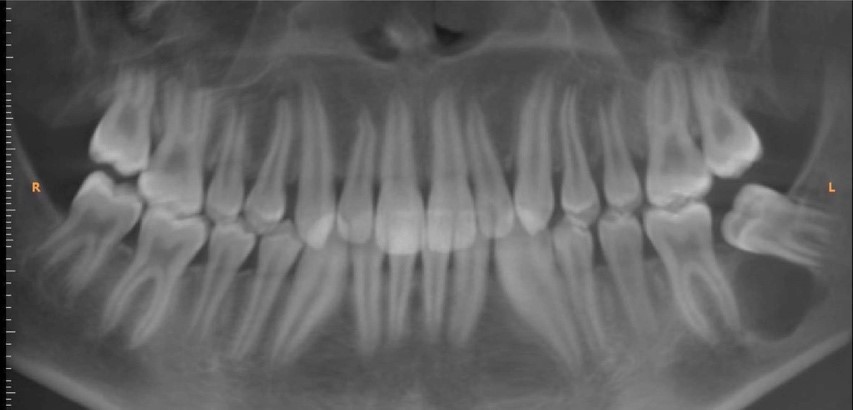
Unilocular radiolucency associated with #18
Histopathologic features
Cystic lesion was lined by thin hyperkeratinizing stratified squamous epithelium. There was no evidence of nuclear palisading and hyperchromatism in the basal cell layer. The lumen contained abundant keratin. The wall was composed of dense collagen and inflammation was unremarkable.
Diagnosis
Orthokeratinized Cyst
Treatment
Surgical enucleation
2nd Case
A 73 year old male presented with a unilocular radiolucency in the area of teeth #14 and 15. (courtesy of Dr. Brett Voegele, Oral Surgeon)
Histopathologic features
This cystic lesion was lined by thin hyperkeratinizing stratified squamous epithelium. There was no evidence of nuclear palisading and hyperchromatism in the basal cell layer. The lumen contained keratin. The wall was composed of dense collagen and inflammation was unremarkable. Interestingly, this cyst had direct connection to the surface epithelium.
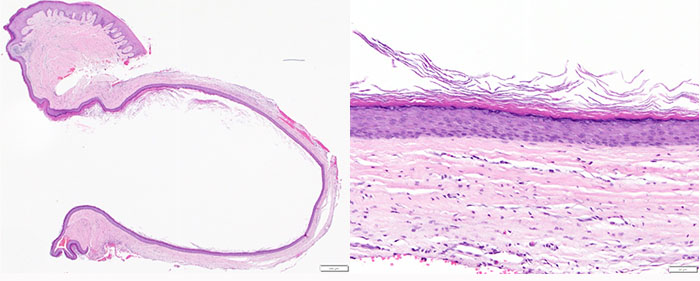
Discussion
The designation of an odontogenic cyst as orthokeratinized is reserved for those jaw cysts characterized by orthokeratinized odontogenic epithelium, partially or in total. In the past, these lesions were classified as odontogenic keratocysts, orthokeratinized type. However they are definitely different, clinicopathologically, from keratocystic odontogenic tumor (KOT; aka odontogenic keratocyst).
They account for about 1% of all odontogenic cysts, the mandible is by far more frequently affected, and they are more common in males. Importantly, their recurrence rate is less than 2% according to studies, compared to KOT 30% recurrence rate.
They may be noticed as an incidental finding and they can be associated with impacted teeth. Differentiating them from dentigerous cysts at the radiographic level is impossible. Generally, they present as unilocular radiolucencies while a multilocular pattern is uncommon. Histologically, the epithelium is hyperkeratinizing with a distinct granular cell layer and no evidence of palisading and hyperchromatism in the basal cell layer and also without a corrugated surface. Keratin production can be seen in both KOT and OOC. Generally, there is no evidence of inflammation in the supporting wall and, if present, it is focal. Occasionally, radicular cysts and dentigerous cysts may exhibit foci of keratinized epithelial lining but this is only focal.
Case #2 is of interest because the cyst lining was connected to the surface epithelium. It is possible in this case that, after extraction, surface epithelium was entrapped in the healing socket and underwent proliferation and cystic changes similar to epidermal inclusion cyst. Alternatively, this cyst may have occupied an area close to the surface and its lining connected to the oral mucosal epithelium.
Palisaded encapsulated neuroma
Clinical History
62-year old male presented with 4 mm painless nodule on the hard palate in the area of the right premolars. (Clinical photograph courtesy of Dr. Troy Alton, Oral Surgeon)

Histopathologic features
Mucosal nodule features well-delineated but unencapsulated peripheral nerve lesion (Figure 1) characterized by intermingling fascicles of Schwann cells in a fibrocollagenous stroma (Figure 2) exhibiting shrinkage or tissue retraction artifact. A delicate perineurium partially surrounds the proliferating fascicles.
Diagnosis
Palisaded encapsulated (solitary circumscribed) neuroma
Treatment
Excisional biopsy.
Discussion
Palisaded encapsulated neuroma is an uncommon oral lesion, however, it is frequent among oral peripheral nerve sheath tumors. It appears in the literature under two names, palisaded encapsulated neuroma or solitary circumscribed neuroma. Prior to its description as a separate entity, these lesions were categorized either as neurofibromas, schwannomas or traumatic neuromas. Palisaded encapsulated neuromas are only partially encapsulated and palisading is present in the minority of lesions. Thus, the term solitary circumscribed neuroma. However, even this term is not precise because there are reports of multiple confluent lesions. These lesions are described on the skin which is the most common location with the oral mucosa second in frequency.
The vast majority of palisaded encapsulated (solitary circumscribed) neuromas involves the masticatory (palate and gingiva) mucosa followed by the labial mucosa, the tongue and buccal mucosa. Extraorally, the perilabial skin is a frequent location. The histopathologic diagnosis is in the vast majority of cases simple and can be supported by immunohistochemical stains that highlight the presence of Schwann cells, nerve axons, which are plenty, and a partial perineurial envelop.
Lesions are most frequently painless, except if traumatized. Treatment is excisional biopsy and recurrence rate less than 1% according to our study.
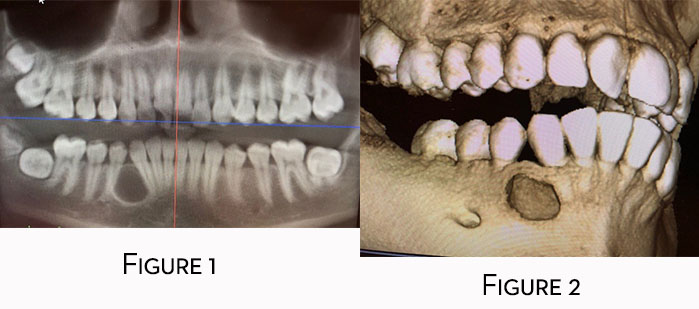
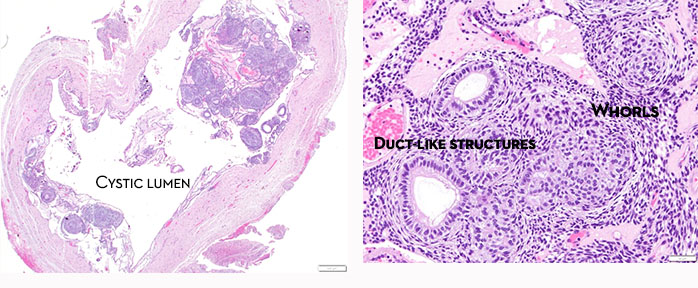
Adenomatoid odontogenic tumor
Clinical History
15-year-old female presented with radiolucent lesion between the lower permanent canine and first premolar with slight expansion of the mandible. The differential diagnosis provided included keratocystic odontogenic tumor (odontogenic keratocyst), ameloblastoma and lateral periodontal cyst (Contributor: Dr. Luke MacMenamin, Oral Surgeon).
Radiographic features
Panoramic radiograph reveals unilocular radiolucency with root divergence (Figure 1). The lesion extended, apparently, through the buccal cortex (Figure 2).
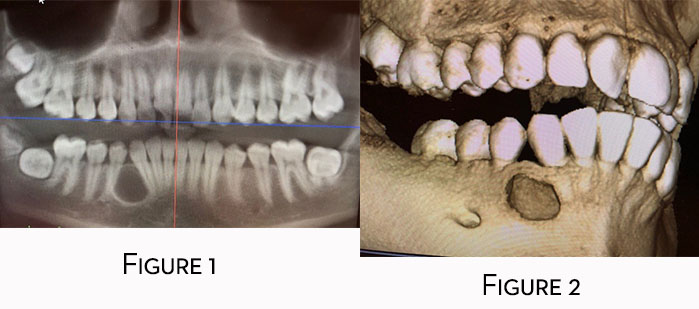
Histopathologic features
Low power microscopy reveals cystic lesion with odontogenic epithelial proliferation into the lumen and along the epithelial lining and formation of small nodules with duct-like structures, rosettes and whorls (Figure 1). Higher power of a representative area reveals whorls of epithelial cells and duct-like structures (Figure 2)
Diagnosis
Adenomatoid odontogenic tumor
Treatment
The lesion was enucleated. No recurrence has been reported.
Discussion
Adenomatoid odontogenic tumor (AOT) is a benign epithelial odontogenic tumor accounting less than 5% of all odontogenic tumors. It occurs, more frequently, in the anterior maxilla. The maxilla is twice more frequently affected than the mandible with strong predilection of the anterior aspect of the jaws. Females are twice more frequently affected than males with 75% of cases occurring in teenagers. Three quarters of the cases are associated with an impacted tooth. Patients are usually asymptomatic and mild expansion may be observed, however, cortical perforation is unusual. Rare extra-osseous examples have been described in the literature.
Radiographically, the lesions are unilocular radiolucencies. Radiopacities may be seen in some cases and are generally small. They represent dystrophic calcifications occasionally present in the tumors. Displacement of teeth and root divergence can be observed; however, root resorption is rare.
A FACTOID TO REMEMBER
The classic presentation of AOT is as a radiolucent or mixed radiolucent/opaque lesion of the anterior maxilla in a teenage girl with impacted canine. A radiographic clue when dealing with an impacted tooth is that the radiolucency in AOT usually starts below the CE junction.
Histopathologically, the lesions are characterized by solid or cystic pattern where one identifies nests exhibiting whorls and rosettes, as well as duct-like structures. The latter finding gives the tumor an adenoid appearance, thus the designation adenomatoid. In the past the tumor was referred to as adenoameloblastoma, however, this term has been abandoned and we discourage its use.
The treatment of choice is enucleation. Recurrence is exceedingly rare.
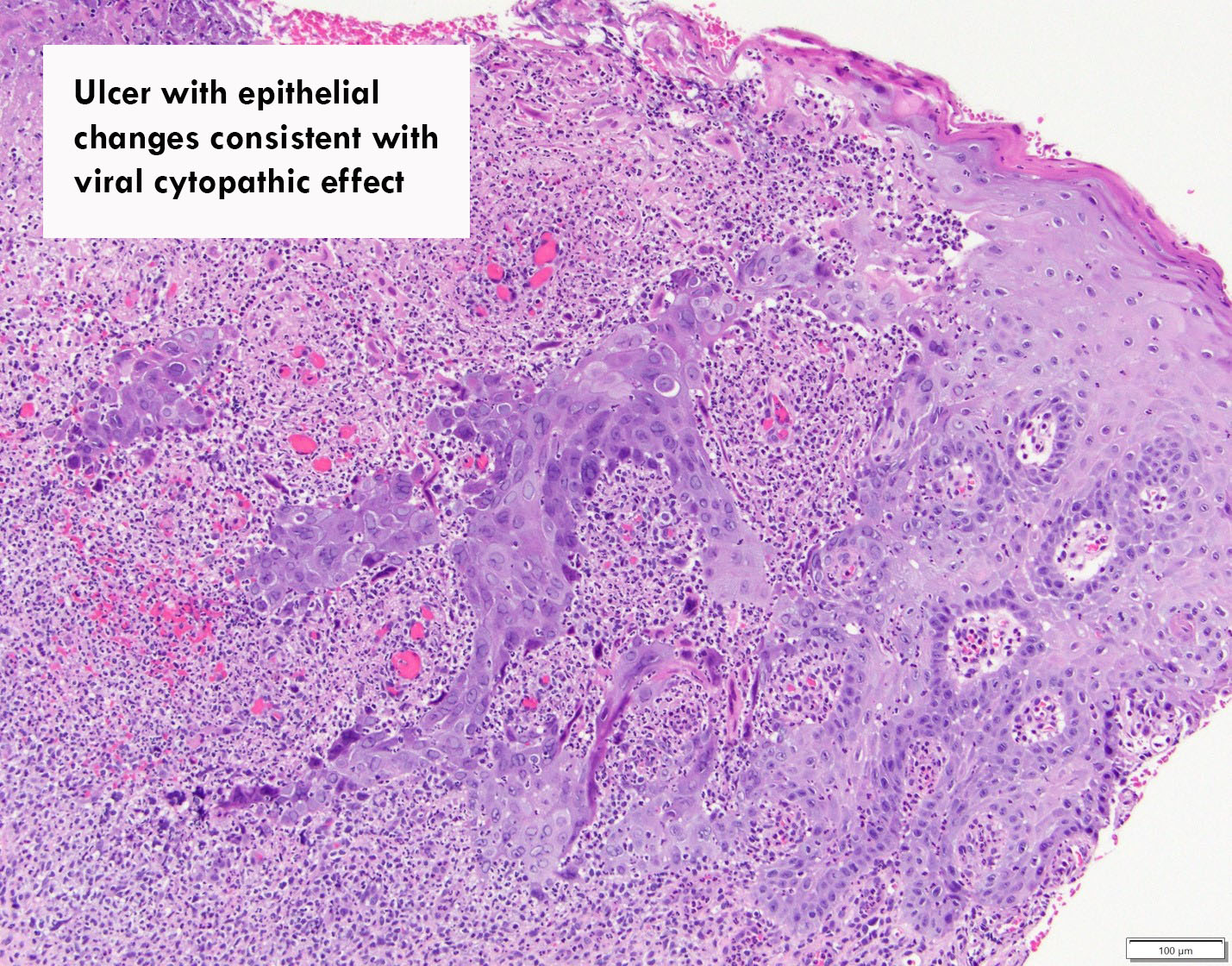
Herpes Simplex
Clinical History
An 80-year-old male presented with multiple ulcers with surrounding erythema preceded by vesicles that coalesced. The patient has polymyalgia rheumatica and had, recently, a flare-up. He was treated by prednisone. (clinical photograph courtesy of Dr. James Block, Oral Surgeon).
Clinical features
Ulcer covered by pseudomembrane with erythematous halo. Smaller erosions or ulcers anteriorly

Histopathologic features
The mucosal fragment was ulcerated and featured so-called cytopathic effect in individual epithelial cells which is related to herpetic infection. Viral inclusion bodies were present in the nuclei of epithelial cells. Immunohistochemistry confirmed the presence of herpes simplex virus infection of the surface epithelium.
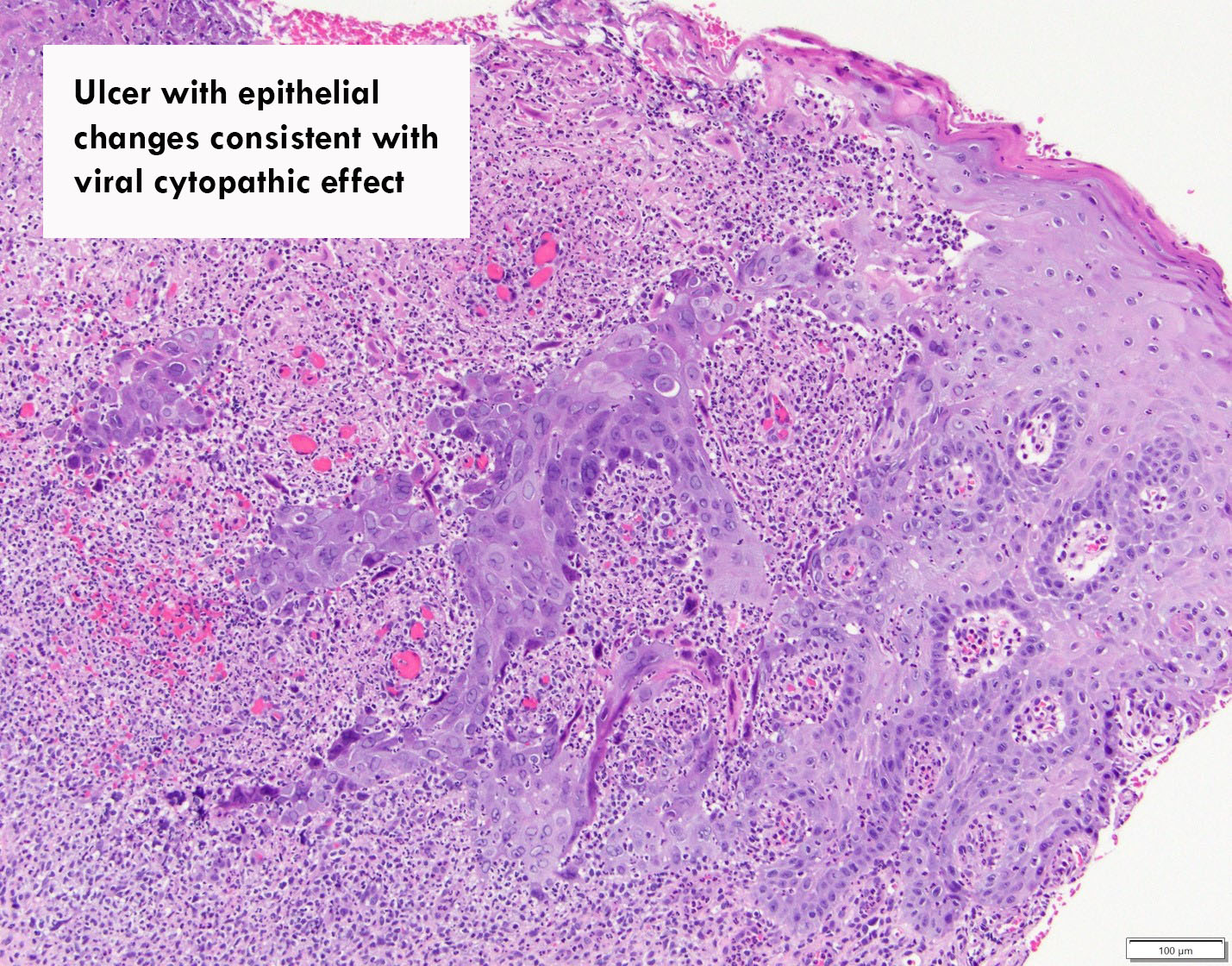
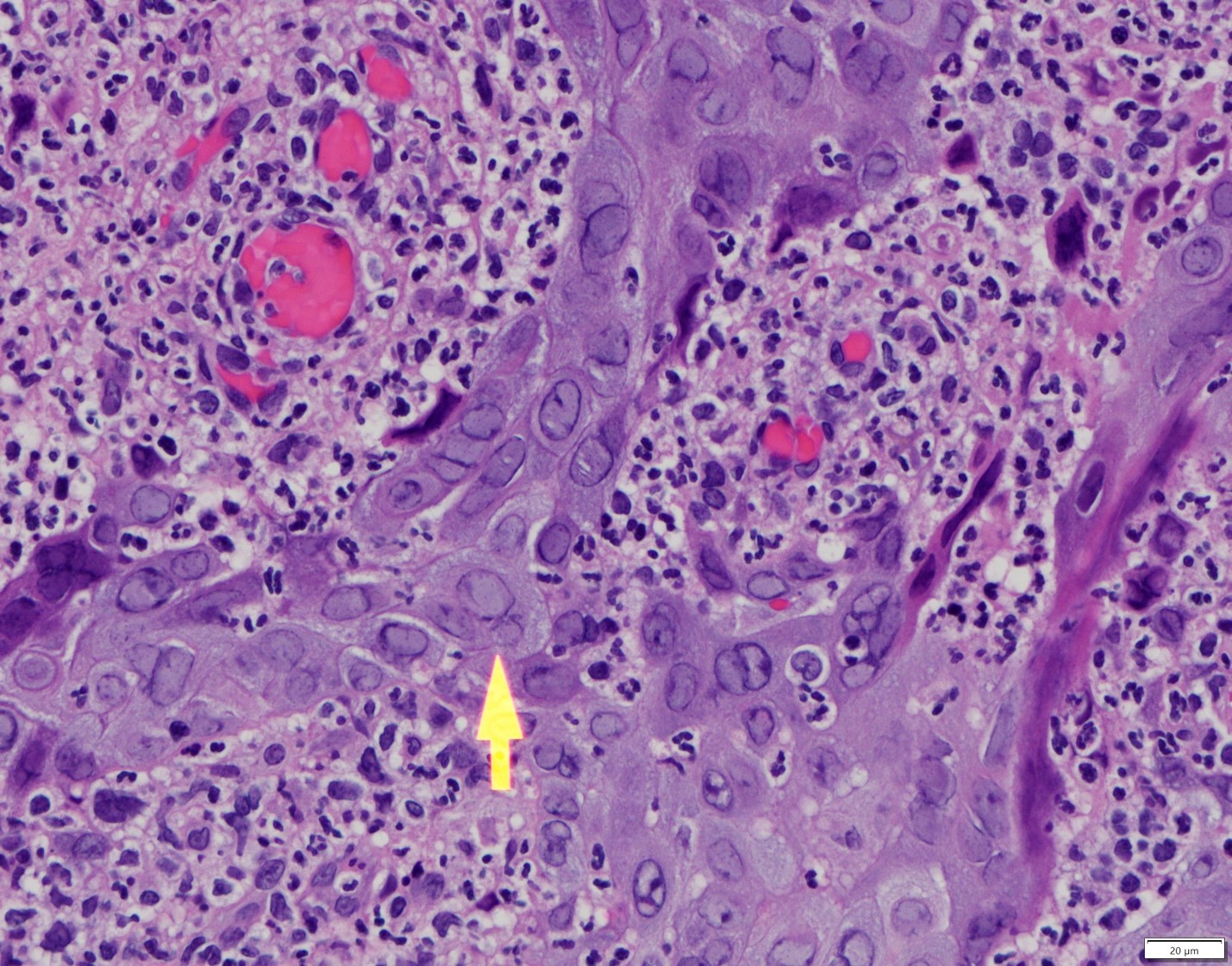
The arrow points to epithelial cells infected by herpes virus. The nucleus is enlarged and has a ground-glass appearance. Other cells feature magenta color nuclei.
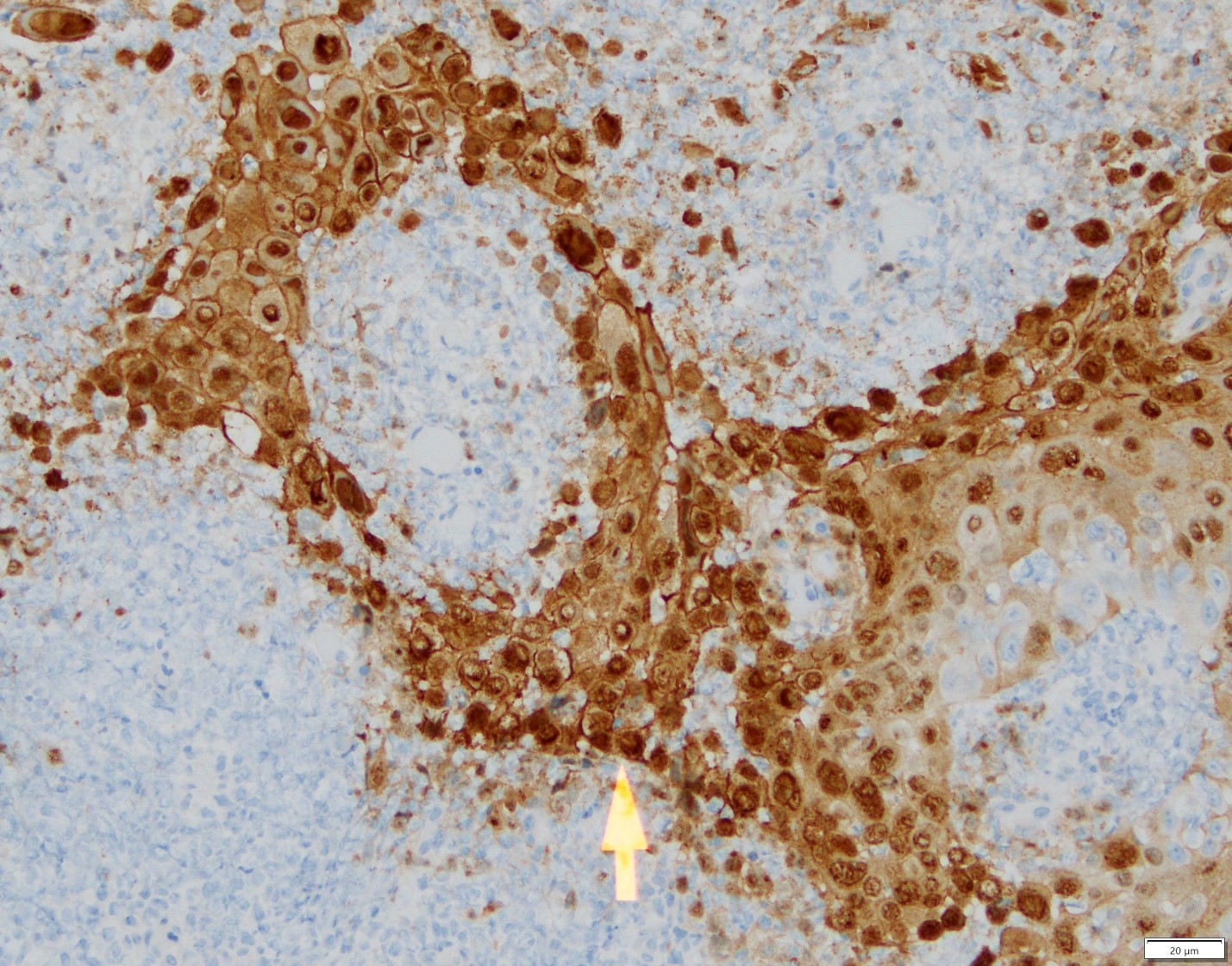
Immunohistochemical evaluation confirmed the presence to herpes simplex virus in individual epithelial cells.
Diagnosis
Ulcer with herpes simplex virus (HSV) cytopathic effect
Treatment
For older patients and patients with recurrent herpes, valacyclovir or famciclovir demonstrate effectiveness and the dosing is convenient for the patients. In patients who present with active lesions such as the case above, tapering off or discontinuation of the immunosuppressive medication may lead to faster resolution of lesions. Certainly, valacyclovir or famciclovir can be used to probably accelerating the healing process. Interestingly, a combination of oral valacyclovir 2 g orally twice daily and clobetasole gel 0.05% twice daily for 3 days can reduce the mean maximum lesion size and mean healing time of classical lesions*.
Discussion
In this particular example, old age and treatment with prednisone can be triggering factors for herpetic infection by herpes simplex virus.
*Hull C, McKeough M, Sebastian K, Kriesel J, Spruance S. Valacyclovir and topical clobetasol gel for the episodic treatment of herpes labialis: a patient-initiated, double-blind, placebo-controlled pilot trial. J Eur Acad Dermatol Venereol. 2009 Mar;23(3):263-7.
Mucoepidermoid carcinoma
Clinical History
A 66-year-old male presented with a firm, mobile lesion on the inner surface of the lower lip opposite to teeth #23 and 24, that was slightly compressible and measuring 0.5x0.5 cm (clinical photograph courtesy of Dr. Nick Spanel, Oral Surgeon).
Histopathologic features
Histopathologic preparation revealed cystic lesion featuring two cavities lined by ductal, squamoid (epidermoid) and, in foci, mucous cells. Mild cytologic variations without mitotic activity were observed. In addition and in deeper sections, predominantly, rare nests of mucous, optically clear and squamoid cells were evident.
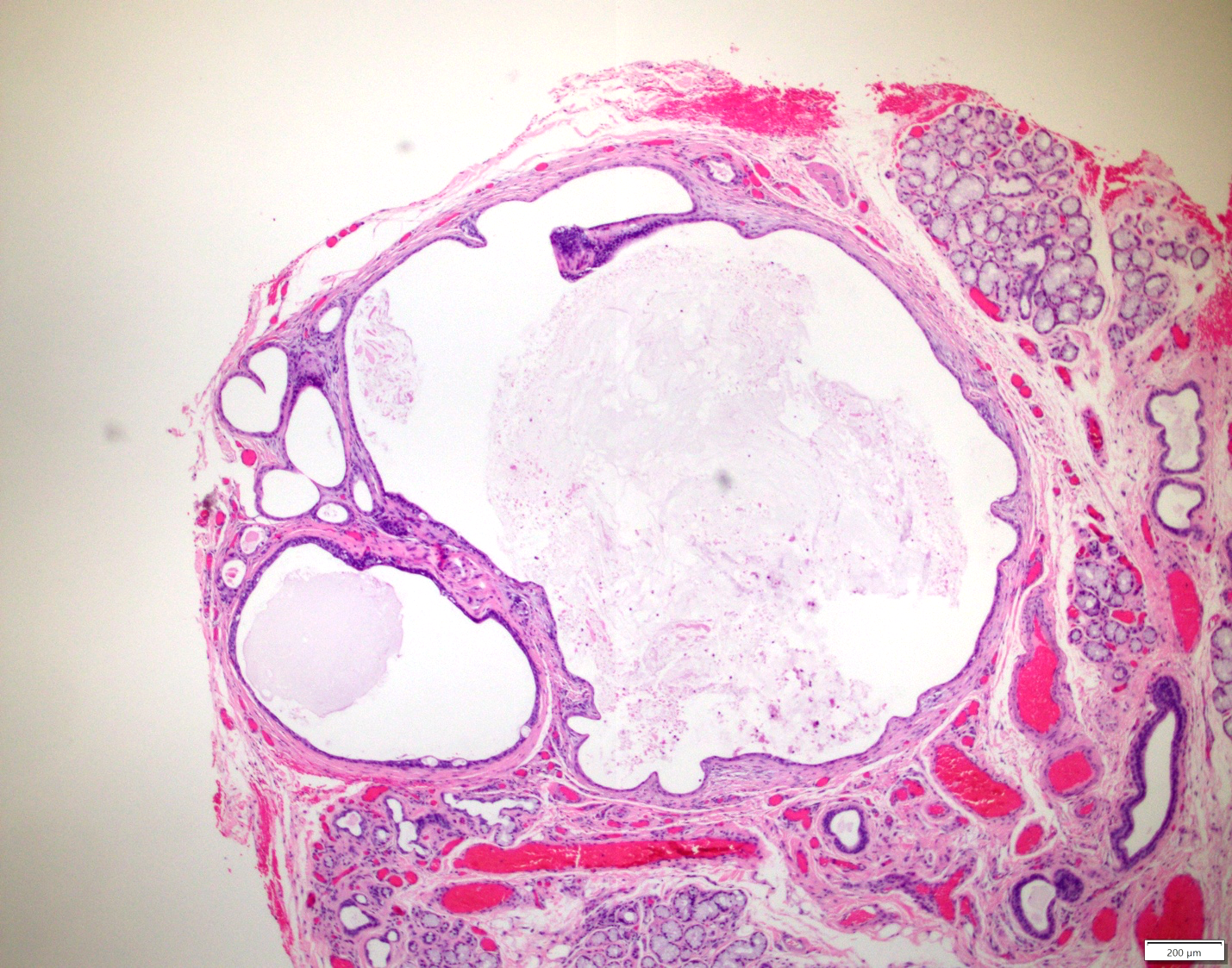
The greatest dimension of the tumor was measured at 2.2 mm. Cavities of various sizes were lined by neoplastic cells.

Diagnosis
Mucoepidermoid carcinoma
Treatment
Excision with tumor free margins is indicated for intraoral tumors. Most frequently intraoral tumors are low-grade and do not metastasize. In the present example, the tumor was contained within the surgical specimen. The patient will be followed.
Discussion
This is one of the smallest examples of mucoepidermoid carcinoma observed in our laboratory. Mucoepidermoid carcinoma is the most frequent malignant salivary glands tumor of major and minor salivary glands. The most frequent location for intraoral mucoepidermoid carcinoma is the posterior hard palate and the soft palate. The lower lip is an uncommon site. The clinical differential diagnosis, given the patient’s age should include salivary gland neoplasia. If trauma is excluded, as a rule, an older individual with a cystic lesion in the lower lip, does NOT have an extravasation type mucocele until proven otherwise. Mucoceles in older individuals are most frequently of the retention type and are seen more frequently in the upper lip.
In the present case, the cells of the neoplastic nests harbored aberrations of a gene known as MAML2. This gene is frequently rearranged in mucoepidermoid carcinomas but not in other malignant salivary gland tumors.
Oral Leukoplakia - Low-grade dysplasia
Clinical History
A 40-year-old male presented with the lesion on the right ventrolateral border of the tongue. The patient is a 15 pack-year smoker. The clinical picture is courtesy of Dr. Troy Alton, Oral Surgeon, Madison, WI.

Histopathologic features
Mucosal fragment was surfaced by hyperparakeratinizing and acanthotic stratified squamous epithelium exhibiting cytologic and architectural variations consistent with low-grade (mild) premalignant epithelial dysplasia.
Discussion
Clinically, the lesion has the characteristics of so-called oral leukoplakia, an oral potentially malignant disorder. According to the World Health Organization, in western countries, the prevalence of leukoplakia generally ranges from 1-4%. Many cases of leukoplakia are associated with tobacco use with or without heavy alcohol consumption. However, some are not and among them few may be related to high risk human papilloma virus (HPV) infection.
Oral leukoplakia is a clinical term used to describe white variations in the oral mucosa that cannot be clinically classified as any other entity. Generally, leukoplakic lesions should be biopsied to evaluate the histologic characteristics of the lesion. Many times leukoplakic lesions are histologically characterized only by epithelial tissue hyperplasia. For the case above, an incisional biopsy was taken and the histology revealed mild (low risk) epithelial dysplasia. Cytologic variations that were interpreted as dysplasia were evident in the lower one third of the surface epithelium.
Sometimes the white plaques of leukoplakia are associated with red (erythematous) areas. In such case the term erythroleukoplakia is used. The presence of a clinical erythematous component increases the possibility of histologic dysplastic changes in the surface epithelium.
In our case after the histopathologic diagnosis was communicated to the clinician, the entire lesion was excised and evaluated for dysplasia-free margins. Interestingly, in the excised specimen, the lesion revealed foci of moderate (high risk) dysplasia in addition to the residual mild dysplasia. The patient is placed on follow-up. Follow-up is important because recurrence may occur and, in some patients, new lesions may arise in other areas.
These lesions include leukoplakia and erythroleukoplakia, the lateral being more frequently associated with dysplasia at the microscopic level.
The interpretation of dysplasia relies on the identification of the following architectural and cytologic abnormal variations
| Architectural | Cytologic |
| Perturbed stratification | Nuclear size |
| Loss of polarity in the basal cell layer | Nuclear shape |
| Mitotic activity in suprabasal areas | Cell size |
| Increased number of mitoses | Cell shape |
| Dyskeratosis; premature keratinization | Nuclear/cytoplasmic ratio |
| Keratin pearls within rete ridges | Atypical mitoses |
| Acantholysis | Increased number and size of nucleoi |
| Abnormal rete ridges; drop-shaped, club-shaped; interconnected, etc... | Nuclear hyperchromatism |
Two different grading systems exist to grade dysplasia. In one, the dysplasia is graded as mild, moderate or severe. The other grading system is binary; low risk and high risk dysplasia, the latter lumping moderate and severe grades. After discussions and review of many histopathologic examples of dysplasia we have decided to use the binary system and this will be implemented this August.
The cut-off point between mild (low-risk) and moderate-severe (high risk) is if four or more architectural and four or more cytologic variations from the list above are observed.
Management of oral premalignant epithelial dysplasia
We suggest the following algorithm when dealing with patients with oral potentially malignant disorder.
Clinical Assessment of the Lesion
- Photography
- Incisional or excisional biopsy
Histopathologic diagnostic possibilities
- Low risk (mild) dysplasia or just epithelial hyperplasia
- If there is clinical concern (non-homogeneous lesion*, lesion size >200 mm2, tongue/floor of mouth location, patient is a smoker, presence of an erythematous component) à resection by a specialist (scalpel or laser); close monitoring of the patient (e.g. one month after the procedure, then every 3 months for the first year, every 6 months the second year and then yearly for at least 5 years to life) by a specialist, i.e. oral surgeon; clinical photography is highly recommended at every appointment..*Rebiopsy may be indicated in cases of non-homogeneous lesions
- If there is no clinical concern (see above) --> monitoring (every 4-6 months) or resection followed by monitoring as above.
- High risk (moderate or severe dysplasia)
- Resection by a specialist and monitoring as above.
Below are two excellent references on the subject of management of oral dysplasia.
- Awadallah M, Idle M, Patel K, and Kademani D. Management update of potentially premalignant oral epithelial lesions. Oral Surg Oral Med Oral Pathol Endo. 2018 Jun;125(6):628-636.
- Field EA, McCarthy CE, Ho MW, Rajlawat BP, Holt D, Rogers SN, Triantafyllou A, Field JK, Shaw RJ. Oral Oncol 2015;51:883-887.
EBV-positive mucocutaneous ulcer
Clinical history
A 64-year old male presented with an ulcerated lesion in the posterior right retromolar mucosa. The patient had heart transplantation. (Clinical photograph courtesy of Dr. Karl Andreasen, Oral Surgeon)

Histopathologic features
Ulcerated lesion revealed proliferation of atypical lymphoid cells harboring Epstein-Barr virus encoding RNA and exhibiting positivity for lymphoid markers CD15 and CD30. The inflammatory population was characterized by B and T cells.
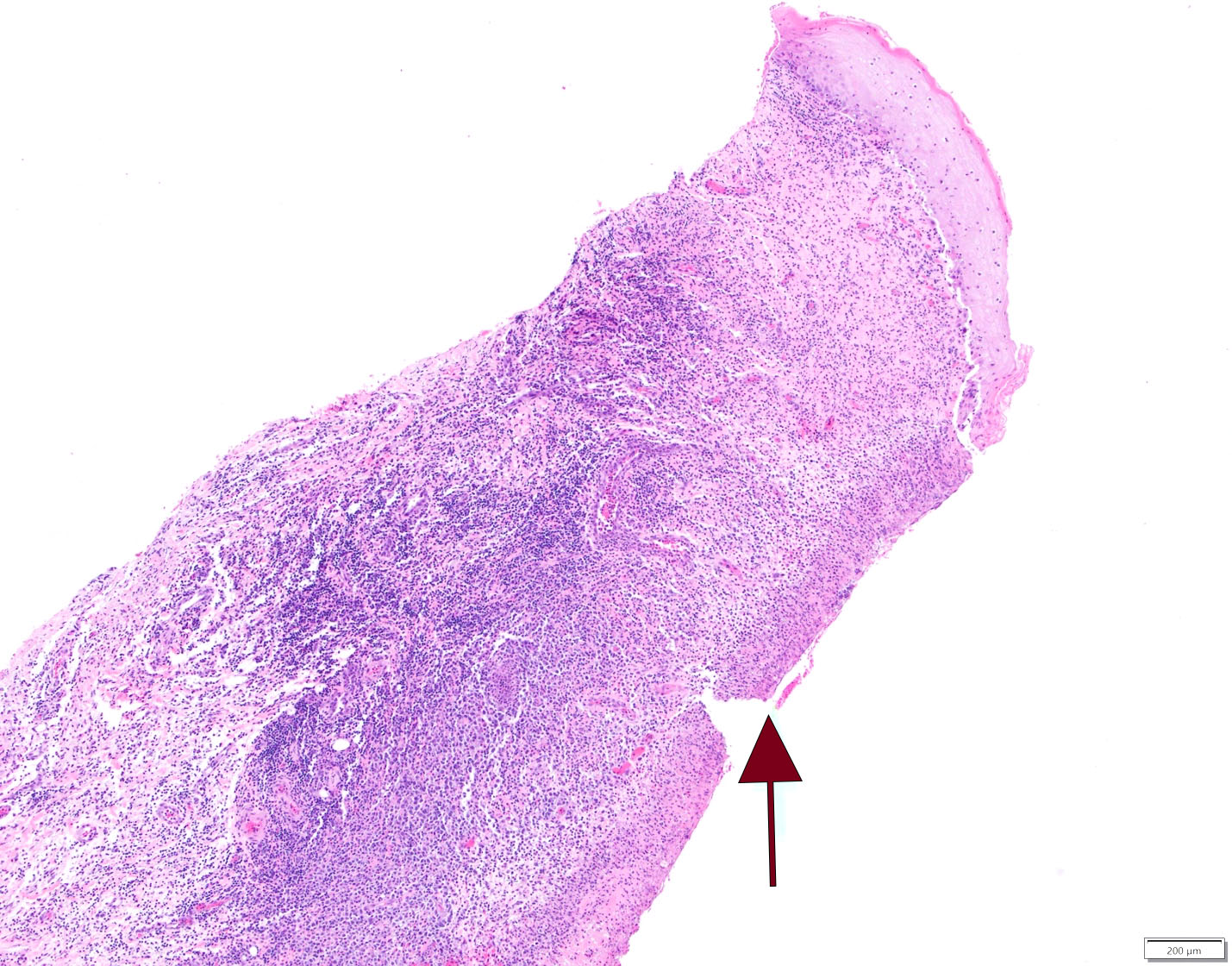
This is an ulcer. The arrow points to the ulcerated surface. At the upper right corner there is a residual surface epithelium.
Atypical lymphoid cells are present in this infiltrate characterized by B and T lymphocytes.

In situ hybridization reaction on the tissue highlights with purple cells harboring Epstein-Barr encoding RNA.
An immunohistochemical stain highlights atypical lymphoid cells exhibiting CD15 positive reaction. CD15 positivity is present in Hodgkin’s lymphoma. However, EBV mucocutaneous ulcers feature also CD15 positive cells.
An immunohistochemical stain highlights atypical lymphoid cells exhibiting CD30 positive reaction. CD30 positivity is present in anaplastic lymphomas and Hodgkin’s lymphoma. However, EBV mucocutaneous ulcers feature also CD30 positive cells.
Diagnosis
EBV-positive mucocutaneous ulcer
Treatment
EBV-positive mucocutaneous ulcer may be the result of advanced age and immunosenescence. Referral to a physician is recommended. For cases in which medication-related immunosuppression is the culprit, the patient should be referred back to his oncologist or transplant surgeon as it was the case with the patient described herein.
If the patient is on immunosuppressive medication, reduction of the dose may lead to complete healing. Those patients for who reduction is not indicated, are treated with monoclonal antibody agents such as rituximab, radiation or other chemotherapeutic agents. A few patients may develop widespread disease or some other form of EBV-positive lymphoproliferative disorder (see below) including lymphoma.
Discussion
Iatrogenic immunosuppression has lead to the development of new pathologic processes affecting occasionally the oral mucosa. One such example is EBV-positive mucocutaneous ulcer. The name implies that these lesions may develop on the skin or mucosal sites including the oral cavity. In many cases EBV-positive mucocutaneous ulcer is related to advanced age. Immunosuppressive medications such as methotrexate, azathioprine, cyclosporine or tumor necrotic factor inhibitors have also been reported as driving factors for the development of such ulcers.
Clinically, oral ulcers may be painful and look aggressive with the clinical differential diagnosis including squamous cell carcinoma. The lesions are many times seen in areas prone to trauma. Besides the mouth and the skin, lesions have been described in the intestinal mucosa.
Oral pathologists are expected to be familiar with these lesions. Careful evaluation of the inflammatory infiltrate and identification of large cells transformed by EBV in association in the presence of intense inflammation can lead to the proper diagnosis which is further confirmed by immunohistochemical stains and in situ hybridization for EBV-encoding RNA. Some cases can resemble lymphoma and sometimes the distinction is very difficult. Also, some cases can look like Hodgkin’s lymphoma (disease) but such neoplasm is very rare in the oral mucosa.